Eduardo P Eyheremendy,1 Andrés J Catalá,1 Federico Orozco Ganem,2 Margarita Anders,2 Patricio Méndez1
1Interventional Radiology Department.
2Liver Transplant Department.
Hospital Alemán, Ciudad Autónoma de Buenos Aires, Argentina.
Acta Gastroenterol Latinoam 2019;49(4):362-366
Recibido: 08/05/2018 / Aprobado: 24/06/2019 / Publicado en www.actagastro.org el 17/12/2019
Summary
Transjugular intrahepatic portosystemic shunt (TIPS) is an established procedure for the secondary prevention of variceal bleeding and management of refractory ascites. Portal vein thrombosis presents technical difficulty during TIPS due to non-visualization of portal vein. In such patients, trans-splenic approach can be utilized to navigate thrombosed portal vein and use a snare as a fluoroscopic guidance for the intra parenchymal pass. The patient had a 2-year history of PVT complicated by abdominal pain, ascites, and paraesophageal varices. The main SV was punctured percutaneous under ultrasound scan guidance. Portal vein (PV) access, PV and Splenic Vein (SV) venoplasty, and TIPS placement were successfully performed without complex techniques. Our case suggests transsplenic (PVR) Portal vein reconstruction-TIPS to be a safe and effective alternative to conventional PVR-TIPS in patients with PVT and SV thrombosis.
Key words. TIPS, trans splenic approach, portal vein thrombosis.
TIPS: abordaje transesplénico en trombosis venosa portal en manejo de ascitis refractaria
Resumen
El shunt hepático portosistémico transyugular (TIPS) es un procedimiento establecido para la prevención secundaria de sangrado variceal y ascitis refractaria. El TIPS, en el contexto de una trombosis venosa portal (TVP), es técnicamente complejo. En tales pacientes, el abordaje transesplénico nos brinda la posibilidad de tener dos canales de trabajo, facilitando el ingreso a la vena porta. El paciente tenía una historia de dos años de TVP complicada con dolor abdominal, ascitis y várices paraesofágicas. Se accedió a la vena esplénica (VE) principal punzándola por vía ecográfica. El acceso a la vena porta (VP), la venoplastía de la VP y de la VE, como así la colocación del TIPS fueron exitosamente realizadas y sin complicaciones técnicas. Nuestro caso expone que la reconstrucción de la vena porta (RVP)-TIPS con abordaje transesplénico es una alternativa segura y efectiva a la RVP-TIPS convencional en pacientes con TVP y trombosis de la VE.
Palabras claves. TIPS, abordaje transesplénico, trombosis venosa portal.
Portal vein thrombosis (PVT) was first reported in 1868 by Balfour and Stewart.1 Among patients with cirrhosis, PVT is common and associated with the severity of patient liver disease.2 Risk of variceal bleeding increases and portal vein access can be difficult in this scenario. Various approaches including trans hepatic, trans-splenic approach, and trans mesenteric ileocolic vein have been utilized to create TIPS in patients with portal vein thrombosis.3
We present the case of a 69-year old patient where we performed a transsplenic approach.
Clinical history
A 69-year-old female patient was diagnosed with cirrhosis due to autoimmune hepatitis, with a history of several episodes of variceal bleeding which was resolved with propranolol and endoscopic treatment. The patient developed an edematous ascites syndrome refractory to medical treatment and a type 2 hepatorenal syndrome with a 1.4mg/dl basal creatinine level. Physical examination showed flapping and instability, edema of lower limbs 3/6, saturation of O2 99%, FC: 79/min, TA: 120/80 and moderate ascites. Medication: propranolol 40 mg, omeprazole 20 mg, spironolactone 200 mg, furosemide 40 mg and folic acid 5 mg.
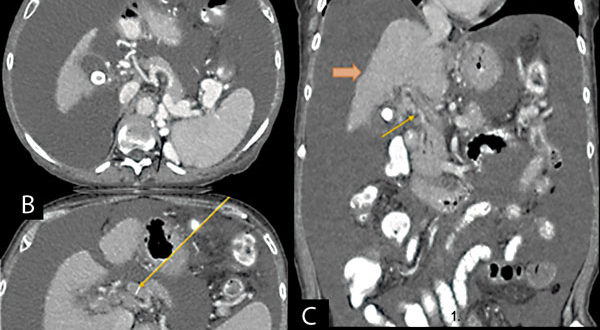
US Color Doppler and CT revealed portal, splenic and mesenteric thrombosis, therefore anticoagulation therapy was administered (Figure 1). The patient was on liver transplant waiting list: MELD classification: 13. Child Pugh B8.
Figura 1. A) collateral circulation of spleno-portal axis (narrow black arrow), B) chronic portal thrombosis (long narrow orange arrow), C) cirrhotic liver (thick orange arrow) and marked ascites.
Pre-treatment imaging
CT scan of the abdomen and pelvis with intravenous contrast was performed to assess spleen, liver, and spleno-portal venous axis.
Treatment options/results
The case was evaluated in a multidisciplinary session, where Transplant and Interventional Radiology Department decided to manage intractable ascites a TIPS procedure.
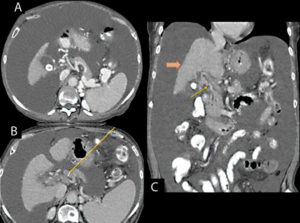
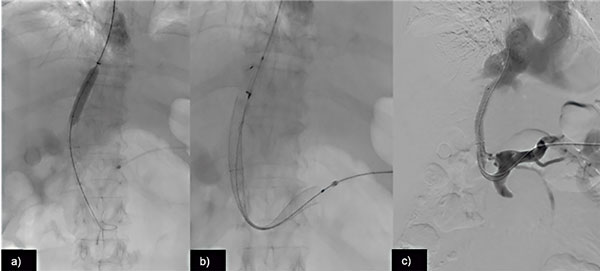
Prior to the beginning, under ultrasound guidance, we placed an abdominal multipurpose catheter to drain ascites. To begin, under ultrasound guidance, we performed a trans-splenic approach with D’ Agostino set. Splenic venogram confirmed portal thrombosis with numerous collateral veins. We placed a snare through splenic vein to connect both pathways (Figure 2).
Figura 2. A) Selective catheterization with contrast of right supra-hepatic vein and B) splenic vein approach by transsplenic puncture with us guidance, C) portal-portal staining showing portal thrombosis and portal cavernomatosis.
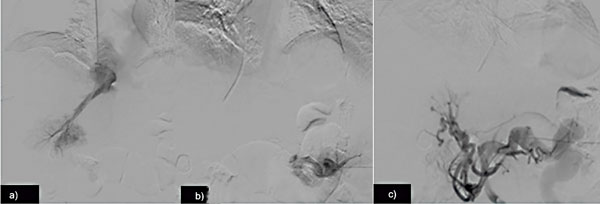
A 9F sheath (Rösch-Uchida Trans jugular Liver Access Set, Cook Medical, Bloomington, Indiana, United States) was inserted via right internal jugular vein under ultrasound guidance. We selectively catheterized right suprahepatic vein with a Cobra catheter and measured portosystemic gradient (20 mm Hg). Then we exchanged the catheter and entered with the metallic sheath, performed and SV road mapping venogram and then intrahepatic puncture with TIPS needle (Figure 3).
Figura 3. A) Right supra-hepatic vein using, B) road mapping to enter portal vein, C) once port-cavo shunt was achieved, a 0.035” Terumo hydrophilic guide is exchanged for Amplatz Superstiff, D) guide was connected from splenic introducer with a metal loop introducer was progressed from supra-hepatic vein to portal circulation, E) portogram was performed and contrast leakage was observed in relation to supra-hepatic puncture (yellow arrow), F) direct portogram after TIPs shows flow with shunt. No intrahepatic portal branches opacification or gastroesophageal varices were diagnosed.
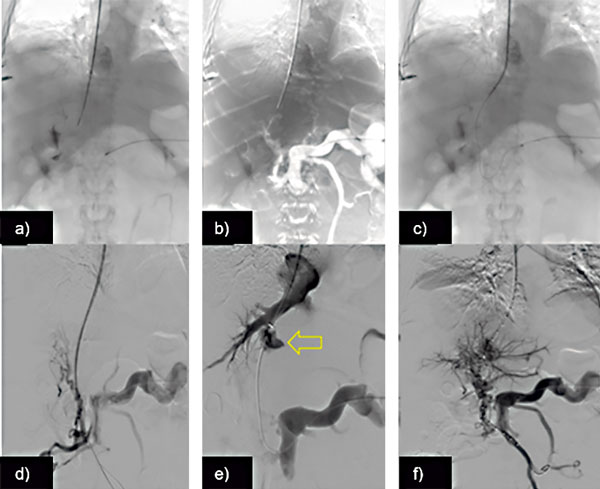
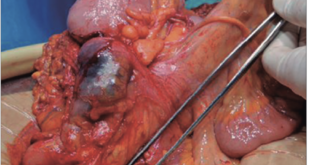
A 60 x 10 mm Viatorr stent (Gore, Newark, DE) was deployed in the liver parenchymal tract, connecting the right PV and the right HV and then a 10 x 94 mm self-expanding wall stent was inserted through splenic vein. Splenic and portal venograms showed good flow through the newly created TIPS and recanalization of the SV and main PV. Portosystemic gradient was 6 mm Hg. We embolized splenic tract with spongostan (Figure 4).
Figura 4. A) Viatorr set and 10 x 60 mm stent covered was progressed. B) Venous portal vein and TIPS with 10 mm x 60 conquest balloon. C) Venography post-angioplasty shows flow restoration in portal vein, superior mesenteric and splenic vein.
Discussion
Portal venous thrombosis (PVT) is a life-threatening complication which may cause or exacerbate and may increase the risk of variceal bleeding and multiorgan failure.4 PVT occurs in 5% – 26% of patients awaiting liver transplant (LT).5 The complexity of portal reconstruction (end to end anastomosis), it worsens LT outcomes.6 PVR-TIPS followed by LT facilitates end-to-end anastomosis, and has a lower incidence of re-thrombosis and gastrointestinal bleeding, and a significantly higher overall survival than nonphysiologic reconstructions.6, 7 However, in patients with PVT, traditional trans jugular PVR-TIPS has a higher failure rate because PV access is more challenging.8
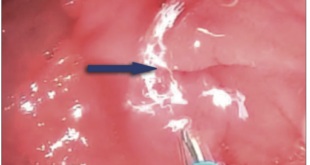
Percutaneous transsplenic PVR-TIPS is an alternative that provides clearer access to the PV in the setting of PVT. Despite improved access, massive hemorrhage, particularly in those with longstanding PH and hematologic derangements, is possible.9 Furthermore; splenic vein (SV) occlusion may nullify the technical advantages of this approach. Although SV was completely occluded, transsplenic PVR-TIPS was a technical success in our patient. SV branches were patent as per USS, allowing for access and venoplasty of the SV without significant impediment. Access and reconstruction of the PV did not require complex techniques, despite the presence of cavernomas.
There were no major hemodynamic complications; however, we were cautious in our technique. In a previous study, Habib et al.7 successfully performed transsplenic PVR-TIPS in 11 patients with cirrhosis-induced chronic PVT. They concluded that, the ideal transsplenic PVR-TIPS candidate is one with main PVT with or without cavernomas. Furthermore, they emphasized the identification of SV access as the most crucial step of the procedure, arguing for US with possible correlation with magnetic resonance imaging. Likewise, our patient had main PVT, and we used US to ascertain SV access. Although the patient required revision of the TIPS, the procedure was uncomplicated. The TIPS remained patent through 2 months of follow-up, however, the patient presented heart failure and died.
Conclusion
Our case suggests that the transsplenic approach to Portal Vein Reconstruction – TIPS is a safe and effective alternative to conventional techniques in patients with portal venous thrombosis and splenic venous thrombosis.
However, patients with more extensive splenic venous thrombosis may not have adequate SV access.
Ergo, more rigorous case series and randomized controlled trials should be conducted to further evaluate its efficacy.
Conflict of interest. There is no conflict of interest.
Financial support. The study was performed without financial support.
Referencias
-
Balfour GW, Stewart TG. Case of enlarged spleen complicated with ascites, both depending upon varicose dilatation and thrombosis of the portal vein. Edinb Med J 1869; 14: 589-598.
-
Amitrano L, Guardascione MA, Brancaccio V. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol 2004; 40: 736.
-
Park J, Kim HC. Transjugular Intrahepatic Portosystemic Shunt Using the Trans-splenic Approach and a Snare Technique. J Clin Interv Radiol ISVIR 2017; 1: 175-178.
-
Ferral H, Bilbao JI. The difficult transjugular intrahepatic portosystemic shunt: alternative techniques and ‘‘tips’’ to successful shunt creation. Semin Intervent Radiol 2005; 22: 300-308.
-
Salsamendi JT, Gortes FJ, Shnayder M, Doshi MH, Fan J, Narayanan G. Transsplenic portal vein reconstruction-transjugular intrahepatic portosystemic shunt in a patient with portal and splenic vein thrombosis. Radiol Case Rep 2016; 11: 186-189.
-
Bilbao JI, Elorz M, Vivas I, Martínez-Cuesta A, Bastarrika G, Benito A. Transjugular intrahepatic portosystemic shunt (TIPS) in the treatment of venous symptomatic chronic portal thrombosis in non-cirrhotic patients. Cardiovascular Intervent. Radiol 2004; 27: 474-480.
-
Chawla YK, Bodh V. Portal vein thrombosis. J Clin Exp Hepatol 2015; 5: 22-40.
-
Hibi T, Nishida S, Levi DM, Selvaggi G, Tekin A, Fan J, Ruiz P, Tzakis AG. When and why portal vein thrombosis matters in liver transplantation; a critical audit of 174 cases. Ann Surg 2014; 259: 760-766.
-
Habib A, Desai K, Hickey R, Thornburg B, Vouche M, Vogelzang RL, Salem R. Portal vein recanalization-transjugularintrahepatic portosystemic shunt using the transsplenic approach to achieve transplant candidacy in patient with chronic portal vein thrombosis. J Vasc Interv Radiol 2015; 26: 499-506.
Correspondencia: Patricio Méndez
Av. Pueyrredón 1640 (C1118 AAT). Department of Interventional Radiology, Hospital Alemán. Ciudad Autónoma de Buenos Aires,
Argentina / Tel.: +54 11 4827-7000
Correo electrónico: pmendez@hospitalaleman.com
Acta Gastroenterol Latinoam 2019;49(4):362-366
 Revista ACTA Órgano Oficial de SAGE
Revista ACTA Órgano Oficial de SAGE