Nicolás González,1 Adolfo Parra-Blanco,2 Vitor Arantes,3 Klaus Mönkemüller4
1 Department of Gastroenterology (Prof Henry Cohen), Hospital de Clínicas, School of Medicine. Montevideo, Uruguay.
2 Department of Gastroenterology, Pontificia Universidad Católica de Chile School of Medicine. Santiago, Chile.
3 Department of Gastroenterology, School of Medicine, Federal University of Minas Gerais. Belo Horizonte, Brazil.
4 Division of Gastroenterology and Hepatology, Basil I Hirschowitz Endoscopic Center of Excellence, University of Alabama. Birmingham, United States.
Acta Gastroenterol Latinoam 2016;46: 213-219
Recibido: 29/12/2015 / Aprobado: 18/04/2016 / Publicado en www.actagastro.org el 03/10/2016
Collaborators
Walton Albuquerque (Brasil), Andrés Donoso Durante (Chile), Walther Bejarano (Colombia), Denny Javier Castro (Venezuela), Rodrigo Castaño (Colombia), Alfonso Calvo (Chile), Sergio Con (Costa Rica), Ricardo Fiszerowicz (Argentina), Jorge Landaeta (Venezuela), Fauze Maluf Filho (Brasil), Daniela Medeiros Milhomem Cardoso (Brasil), John Ospina Nieto (Colombia), Arecio Peñaloza-Ramírez (Colombia), Raúl Pinilla (Colombia), Lix Alfredo Reis de Oliveira (Brasil), Mario Rey Ferro (Colombia), Carlos Antonio Robles Medranda (Ecuador), María Constanza Rodríguez Rubiano (Colombia), Paulo Sakai (Brasil), Gloria Vargas Cárdenas (Perú), Guido Villa-Gómez (Bolivia), Nancy Zambrano H (Venezuela).
Summary
Endoscopic submucosal dissection (ESD) has been performed routinely in Asia for many years, however, in Western countries ESD it is still limited to a few tertiary centers. Objectives. To investigate the practice of ESD in Latin America. Methods. An electronic survey was mailed to Latin-American endoscopists affiliated with National Societies of Gastroenterology and Endoscopy under the collaboration of the Interamerican Association of Gastroenterology and the Interamerican Society of Digestive Endoscopy. Endoscopists from Latin America with publications related to ESD until May 2013 were also invited to participate. Results. A total of 37 endoscopists completed the survey, 25 (67%) performed ESD in humans (ESDH). ESDH was performed in 23 centers located in 10 out of 23 countries (43%). A total of 23 operators of ESDH (92%) had previously been trained in animal models performing 936 ESD. A total of 723 ESDH were performed: stomach 62%, esophagus 15%, colorectum 22%. The average number of procedures per endoscopist was 29 (range: 1-73).There were 9.2% complications (4% perforations, 4.5% postoperative bleedings and 0.7% miscellaneous). Conclusions. Although the number of endoscopists in Latin America performing ESD is still relatively low, the number of ESDH being performed is significant. The vast majority of operators appear to have received proper training in pig models and attended Japanese referral centers. The outcomes appear to be similar to Eastern publications.
Key words. Endoscopic submucosal dissection, training, learning curve, endoscopic mucosal resection, endoscopic resection.
Situación Actual de la disección endoscópica de la submucosa en América Latina
Resumen
La disección endoscópica de la submucosa (ESD) se realiza de forma rutinaria en Asia desde hace muchos años; sin embargo, en los países occidentales la práctica de la ESD todavía se limita a unos pocos centros. Objetivos. Conocer la práctica de la ESD en América Latina. Métodos. Una encuesta electrónica fue enviada por correo a los endoscopistas latinoamericanos afiliados a las Sociedades Nacionales de Gastroenterología y Endoscopia con la colaboración de la Asociación Interamericana de Gastroenterología y la Sociedad Interamericana de Endoscopia Digestiva. También se invitó a participar a los endoscopistas de América Latina que tenían publicaciones relacionadas con ESD hasta mayo de 2013. Resultados. Un total de 37 endoscopistas completaron la encuesta, 25 (67%) realizaban ESD en seres humanos (ESDH). ESDH se realizaba en 23 centros ubicados en 10/23 países (43%). Un total de 23 endoscopistas que realizaban ESDH (92%) habían utilizado los modelos animales para su entrenamiento, realizando 936 ESD. Se realizaron 723 ESDH: en estómago 62%, esófago 15%, colon y recto 22%. El número promedio de procedimientos por endoscopista fue de 29 (rango: 1-73). Hubo 9.2% de complicaciones (4% perforaciones, 4,5% hemorragias postoperatorias y 0,7% misceláneas). Conclusiones. A pesar que el número de endoscopistas que realiza ESD en Latinoamérica es todavía relativamente bajo, el número total de procedimientos realizados en humanos ESDH es significativo. La gran mayoría de los operadores parecen haber recibido formación en modelos porcinos y asistido a centros de referencia japoneses. Los resultados parecen ser similares a las publicaciones de países europeos.
Palabras claves. Disección endoscópica de la submucosa, entrenamiento, curva de aprendizaje, resección de la mucosa endoscópica, resección endoscópica.
Abbreviations
ESD: endoscopic submucosal dissection.
ESDH: ESD in humans.
ISI: International Sensitivity Index.
Endoscopic submucosal dissection (ESD) was developed in Japan with the aim of completely resecting neoplastic tumors in one piece and with adequate free margins.1-3 Although, initially ESD was utilized for early gastric cancer, soon afterwards it became evident that early esophageal and superficial colorectal cancer could also be managed effectively using this novel technique. In spite of the excellent results obtained in Japan in terms of effectiveness and safety,4, 5 the use of ESD in Western countries remains limited to a few referral centers. The major drawbacks to incorporation of ESD are several and include a) the perceived low rate of early tumor detection in Western centers, b) its being a complex procedure and c) the steep and long learning curve associated with the procedure. In countries like Japan and South Korea there is a high prevalence of gastric cancer in the population, and the endoscopists are highly skilled to recognize the tumors in early stages.6 The early gastric tumor, particularly when situated in the antrum, is considered the most suitable lesion to be managed by novice ESD operators. Moreover, expert centers in Japan have developed structured training programs for hands-on practice in animal models and training in humans.7 Due to its advantages in terms of potential complete resection, the interest in ESD has grown in Europe.8 In the Americas a similar movement has been observed. However, there is scarce data about the number of endoscopists involved in ESD practice and the outcome of this procedure in such centers. Knowledge of these data is of paramount importance to the further implementation, refinement and establishment of this technique. The present study aimed to investigate the current status of ESD practice in Latin America.
Material and methods
A survey with specific questions on ESD and its practice was developed (Table 1). The survey was elaborated in both Spanish and Portuguese and the following data were requested: identification, type of institution (academic/public/private), medical training background, scientific publications or congress presentations related to ESD, characteristics of training program, experimental hands-on practice in animal models, number and type of procedures performed in humans, devices utilized, adverse events and outcome.
Table 1. Summary of the results of the survey for human ESD.

This survey was electronically mailed to Latin-American endoscopists from 23 countries affiliated with National Societies of Gastroenterology and Endoscopy with the collaboration of the Interamerican Association of Gastroenterology (AIGE) and the Interamerican Society of Digestive Endoscopy (SIED). In order to find all potential individuals performing ESD in Latin America an additional literature search using the PubMed search engine up to the year 2013 was performed.
Statistical analysis
Data are presented in descriptive fashion and variables are summarized in absolute frequencies, percentages, means and/or medians, as needed. The software used was SPSS (version 17.0; SPSS Inc, Chicago, Illinois, USA).
ESD survey results in humans
A total of 37 endoscopists from 23 centers distributed in 10/23 countries (43%) adequately answered and returned the survey and reported to perform ESD. Twenty five (67%) had performed ESD in humans (ESDH), and 12 (33%) only in animal models. Of the endoscopists who had studies published in journals indexed on PubMed, 5/6 (83%) completed the questionnaire.
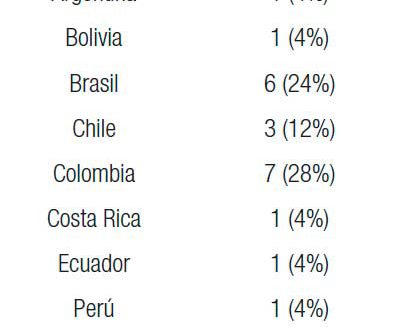
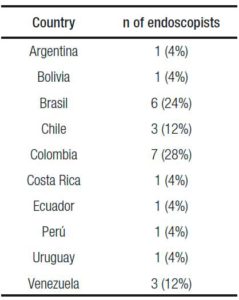
Table 1 shows a summary of the results of the survey for human ESD. The distribution of endoscopists performing ESDH per countries can be seen in Table 2.
Table 2. Distribution of endoscopists performing ESDH per countries.
Practice on animal models had been carried out by 35/37 (95%). Most of the endoscopists who were performing ESDH had also practiced on animal models before embarking on human endoscopic resections 23/25 (92%). The majority (18/25 or 78%) used both ex-vivo and in-vivo models, 4 (17%) only in-vivo models, and 1(4%) only ex-vivo. The porcine model was the choice for all cases (100%), and one endoscopist also used the canine model. Six endoscopists (24%) had an animal laboratory to perform ESD practice in living models. In total, the reported number of procedures performed on animal models previous to attempting ESDH was 936, with a mean 40,7 per endoscopist (3-200). Eight (35%) endoscopists had performed more than 30 procedures in animal models. In addition most of the endoscopists (21/25: 84%) performing ESDH had visited referral training centers.
The following knives were used: IT- knife 18 (72%), Flush knife 12 (48%), Flex knife 5 (20%), Hook knife 5 (20%), Hybrid knife 3 (12%), Dual knife 3 (12%), Triangle knife 2 (8%). Five endoscopists (20%) had used only one type of knife, 13 (52%) had used two, 4 (16%) had used three, and 3 (12%) had used four.
A total of 723 ESDH were performed: 62% in the stomach, 15% in the esophagus, 15% in the rectum and 7% in the colon (Table 1). The median number of procedures per endoscopist was 29 (1-73). Ten endoscopists (40%) had performed at least 30 ESDH.
Fourteen respondents (56%) were the only endoscopists performing ESDH at their center, eight (32%) reported having two endoscopists performing, and 3 (12%) answered that there were 3 endoscopists in their institution performing ESDH.
Major complications (perforation or bleeding) were reported by 21 (84%) endoscopists. The total number of complications was 68 (9.4%), 30 (44%) were perforations, 33 (48%) bleeding, and 5 (7%) were other complications. There was one fatal complication due to bleeding (0.09%). Among the major complications, 65% were treated endoscopically, 17% required surgery and there were no data on the remaining 18%.
Among the endoscopists performing ESDH, 10 (40%) had publications on this technique in scientific journals and 6 (24%) in journals indexed in PubMed. The total number of articles published in scientific journals was 32, of whom 16 (50%) were indexed in PubMed.10-29
Discussion
This is the first report evaluating the prevalence and utilization of ESD in Latin America. The survey indicates that ESD has definitely arrived to the American continent and is being performed in at least 43% (10/23) of the countries. Even though the number of endoscopists performing ESD can be considered relatively low, with only 25 individuals reporting on ESDH, the number of reported cases performed is high. Indeed, the mean number of ESD performed by Latin American endoscopists was higher than the number reported by the European ESD survey (29 versus 11).8 It is possible that this larger number reflects the larger number of gastric cancers in some Latin American countries. Nonetheless, 35% of ESDs reported involved the colorectum and esophagus. Thus, it appears that Latin American endoscopists have adopted this technique for lesions of the entire GI tract. In addition, colorectal lesions with an indication for ESD can be a frequent finding in countries such as Uruguay, where the incidence of colorectal cancer is high, and a national screening program exists.
This survey also stands out for having evaluated two additional issues, both of which may have an influence on the quality of practice of ESD: a) previous training and b) publication of results in scientific journals. An interesting finding was that the vast majority of endoscopists performing ESDH had previously trained using live or inanimate biologic models and visited expert centers in Japan. These results are encouraging as they reflect a willingness to adopt this method under ideal circumstances. Often times, new techniques fail or are abandoned due to improper training.9 It is striking to see that Latin American endoscopists performing ESDH had trained on almost 1000 pig stomach resections before attempting this technique in humans. While it is impossible to know from this survey if other endoscopists performing ESDH who did not respond to the questionnaire had an adequate training as well, we believe that this aspect of previous training must be emphasized as a prerequisite for embarking in ESD. ESD is technically demanding and requires a lot of practice to achieve competence. For these reasons, training programs have been developed in different American countries using porcine models, and frequently including Japanese experts as trainers. It has been shown that these courses may help improve the skills in this technique in a relatively short time.7
An additional finding of the current survey was that a significant percentage of Latin American endoscopists reported an interest in making their experience available by publishing the results in peer review journals.10-29 Previous surveys have not evaluated this aspect, which we believe is important as any adoption of new technique should lead to publication of positive or negative results.
ESD is still not a widespread technique outside Japan, Korea and China. Nonetheless, it is clear that ESD allows “en bloc” resection of superficial neoplastic lesions, almost without any size limit. Its spread in Western countries has been limited, probably because of the technical difficulties and the initial higher risk of complications. However, in experienced hands ESD results in lower complications. The most frequent major complications reported in this study were bleeding (4.5%), and perforation (4%). These results are not different from those obtained in Asian referral centers, which reported complication rates of 1-4%.30 The results from the European survey previously mentioned reported over 8% bleedings, and 5% perforations.8 Therefore, it could be concluded that the rate of complications by Latin American endoscopists who completed the survey was slightly lower than those reported by western endoscopists.
ESD is a technically demanding method, and certainly not every therapeutic endoscopist should be expected to perform it. Moreover, the number of lesions with a clear indication for ESD in Latin American slow, perhaps explaining the reduced number of expert endoscopists practicing this technique in each country. This approach is supported by results of a previous survey of Japanese experts in colorectal ESD.30 It is encouraging to observe that Latin American endoscopists performing ESDH have gone through a process of training before embarking in human ESD. Regarding the number of ESDs performed per endoscopist in the different gastrointestinal locations (esophagus, stomach, colorectum) the mean number was 29, and 40% of the endoscopists performed at least 30 procedures, and 24% performed at least 40 cases. Gotoda et al,7 and Kakushima et al32 suggested that at least 30 gastric ESDs supervised by an expert were required for the beginner to gain competence in this technique. Choi et al,33 reported that 20-40 procedures would be the ideal number to achieve initial competence, considering safety and effectiveness. However, in a recent study Yamamoto et al34 suggested that 30 procedures is an insufficient number to achieve competence in ESD of gastric lesions in any location, and according to another study by the same authors, 40-80 procedures would be required to achieve competence, and over 80 to be able to resect safely and with efficacy lesions of any location.35 Therefore, if the algorithms suggested by the Japanese experts about the learning curve are considered and applied, it can be stated that the number of endoscopists with enough experience is low. Similarly, Dinis- Ribeiro et al36 recommend having performed 20-40 ESD initially in the distal stomach and later in proximal locations before starting to practice esophageal and colorectal ESD. Ohata et al37 propose that at least 30 gastric ESD would be required to achieve enough competence to start colon ESD. However, other recent studies suggest that it would not be necessary to have a lot of competence in gastric dissections before being able to perform colon ESD.38 The number of endoscopists performing human ESD per center was also analyzed. The low number of endsocopists performing ESD per center can be related to the low number of lesions treated per institution, as well as the recommendation from experts in that field that one endoscopist acquire initial experience before starting the training of a second endoscopist, so that the first can become the trainer of the second.31
With the results obtained in this survey, and considering that ESD is effective and safe in expert hands, the authors consider that well-structured training programs would be required in Latin America and Western countries in general, to increase the implementation of ESD. Such courses should include animal models, with the supervision of experts, and this should be complemented by visits to referral centers. The authors believe that these programs should focus also in the detection and evaluation of early digestive neoplasms and should be adapted to the needs and possibilities of each region.
We would like to acknowledge the limitations of this study. Any survey study has the potential limitation of inaccuracy of the data, as the reported results are retrospective, not always based on registries and some endoscopists performing ESD may not have received the survey or did not answer the survey. In spite of this, we know that the vast majority of endoscopists who had publications in PubMed responded to the questionnaire. One other limitation we must mention is that the results of the procedures were not obtained (en bloc resection rates, R0 resection rates), as this was not the objective of this study and the survey did not include questions related to this topic. Nevertheless, our survey provides new findings not addressed by previous survey studies, such as the importance of using animal models when practicing this technique and the percentage of endoscopists who have publications in indexed journals.
In summary, this study allows for important conclusions regarding ESDH in Latin America. We found that ESD is performed in 40% of Latin American countries. Although the number of endoscopists in Latin America performing ESD is still relatively low, the number of ESD is significant. The great majority of operators appeared to have received proper hands-on training in biologic models and attended Japanese referral centers before embarking on ESDH. Despite not knowing the remedial results of these procedures, the reported outcomes in terms of complications and mortality rates appear to be similar to Eastern and European publications.
Our findings support the creation of a closer collaboration among the different Latin American centers, with the aim of creating working groups which promote and participate in teaching, research and developing this technique in depth. Forming close relationships with Asian centers and other Western countries is also considered of great importance to achieve technical improvement and allow for clinical application. All these actions should facilitate the smooth introduction and development of ESD, attracting the interest of the companies related to ESD devices and making them understand that it is a useful technique. This is appealing to endoscopists but especially important to patients, so that the armamentarium available for ESD in Japan is also made available to Latin American endoscopists.
Acknowledgements. The authors wish to thank: Gastroenterology and Endoscopy Societies of Latin American countries and American Gastroenterological Association (AIGE) and Inter American Society of Endoscopy (SIED) for facilitating access of their members to the survey. We also want to thank Dr Carlos Reolon for his contribution designing the electronic questionnaire.
Referencias
- Oyama T, Tomori A, Hotta K, Morita S, Kominato K, Tanaka M, Miyata Y. Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol 2005; 3: S67-S70.
- Yamamoto H. Endoscopic submucosal dissection of early cancers and large flat adenomas. Clin Gastroenterol Hepatol 2005; 3: S74-S76.
- Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut 2001; 48: 225-229.
- Muto M, Miyamoto S, Hosokawa A, Doi T, Ohtsu A, Yoshida S, Endo Y, Hosokawa K, Saito D, Shim CS, Gossner L. Endoscopic mucosal resection in the stomach using the insulated-tip needle-knife. Endoscopy 2005; 37: 178-182.
- Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 2010; 72: 1217-1225.
- Gotoda T. Endoscopic resection for premalignant and malignant lesions of the gastrointestinal tract from the esophagus to the colon. Gastrointest Endosc Clin N Am 2008; 18: 435-450.
- Gotoda T, Friedland S, Hamanaka H, Soetikno R. A learning curve for advanced endoscopic resection. Gastrointest Endosc 2005; 62: 866-867.
- Ribeiro-Mourão F, Pimentel-Nunes P, Dinis-Ribeiro M. Endoscopic submucosal dissection for gastric lesions: results of an European inquiry. Endoscopy 2010; 42: 814-819.
- Fry LC, Mönkemüller K, Malfertheiner P. Systematic review: endoluminal therapy for gastro-oesophageal reflux disease: evidence from clinical trials. Eur J Gastroenterol Hepatol 2007; 19: 1125–1139
- Tanimoto MA, Torres-Villalobos G, Fujita R,Santillan-Doherty P, Albores-Saavedra J, Gutierrez G, Martin-del-Campo LA, Bravo-Reyna C, Villanueva O, Villalobos JJ, Uribe M, Valdovinos MA. Endoscopic submucosal dissection in dogs in a World Gastroenterology Organisation training center. World J Gastroenterol 2010; 16: 1759-1764.
- Chaves DM, Maluf Filho F, de Moura EG, Santos ME, Arrais LR, Kawaguti F, Sakai P. Endoscopic submucosal dissection for the treatment of early esophageal and gastric cancer-initial experience of a western center. Clinics (Sao Paulo) 2010; 65: 377-382.
- Chaves DM, Moura EG, Milhomem D, Arantes VN, Yamazaki K, Maluf F, Albuquerque W, Conrado AC, Araújo JC, Uejo PH, Sakai P. Initial experience of endoscopic submucosal dissection in Brazil to treat early gastric and esophagheal cancer: a multi-institutional analysis. Arq Gastroenterol 2013; 50: 148-152.
- Vargas C G, Chávez R M, Sanchez V, Rojas R P, Verona R R.Therapy for early gastric cancer with submucosal endoscopic dissection using the IT-Knife 2. Rev Gastroenterol Perú 2012; 32: 297-302.
- Tanimoto MA, Torres-Villalobos G, Albores-Saavedra J. Endoscopic submucosal dissection of a colonic tubulovillous adenoma with high grade dysplasia. Rev Gastroenterol Mex 2011; 76: 50-51.
- Con SA, Con-Chin GR, Kishimoto G, Con-Wong R. Endoscopic submucosal dissection (esd) for the curative treatment of early gastric cancer: initial experience in Costa Rica. Rev Gastroenterol Peru 2009; 29: 276-280.
- Con SA, Kishimoto G, Con-Chin GR, Con-Wong R. Advances in surgical endoscopy: initial experience in endoscopic colonic submucosal dissection (ESD) in Costa Rica. Rev Gastroenterol Peru 2012; 32: 79-83.
- Con SA, Saito Y, Matsuda T, Taniguchi H, Nakajima T. Application of endoscopic submucosal dissection for removal of deep invasive submucosal colon carcinoma. Case Rep Med 2009; 2009: 573981.
- Con SA, Oda I, Suzuki H, Kusano C, Kiriyama S, Gotoda T. Risk of perforation during endoscopic submucosal dissection using latest insulation-tipped diathermic knife (IT knife-2). Endoscopy 2009; 41: E69-E70.
- Wang AY, Emura F, Oda I, Cox DG, Kim HS, Yeaton P. Endoscopic submucosal dissection with electrosurgical knives in a patient on aspirin therapy (with video). Gastrointest Endosc 2010; 72: 1066-1071.
- Santos JO, Miyajima N, Carvalho R, Leal RF, Ayrizomo M de L, Coy CS. Feasibility of endoscopic submucosal dissection for gastric and colorectal lesions: Initial experience from the Gastrocentro – UNICAMP. Clinics (Sao Paulo) 2013; 68: 141-145.
- Cardoso DM, Campoli PM, Yokoi C, Ejima FH, Barreto PA, de Brito AM, Mota ED, de Fraga Júnior AC, da Mota OM. Initial experience in Brazil with endoscopic submucosal dissection for early gastric cancer using insulation-tipped knife: a safety and feasibility study. Gastric Cancer 2008; 11: 226-232.
- Kawaguti FS, Nahas CS, Marques CF, Martins BC, Retes FA, Medeiros RS, Hayashi T, Wada Y, de Lima MS, Uemura RS, Nahas SC, Kudo SE, Maluf-Filho F. Endoscopic submucosal dissection versus transanal endoscopic microsurgery for the treatment of early rectal cancer. Surg Endosc 2014; 28: 1173-1179.
- Parra-Blanco A, Arnau MR, Nicolás-Pérez D, Gimeno-García AZ, González N, Díaz-Acosta JA, Jiménez A, Quintero E. Endoscopic submucosal dissection training with pig models in a Western country. World J Gastroenterol 2010; 16: 2895-2900.
- Parra-Blanco A, Gonzalez N, Rosa Arnau M. Review on ex-vivo and in-vivo models for ESD training. Clinical Endoscopy 2012; 45: 350-357.
- Arantes V, Albuquerque W, Freitas Dias CA, Demas Alvares Cabral MM, Yamamoto H. Standarized endoscopic submucosal tunnel dissection for management of early esophageal tumors (with video). Gastrointest Endosc 2013; 78: 946-952.
- Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Fu KI, Sano Y, Saito D. Endoscopic treatment of large superficial colorectal tumors: a case series of 200 endoscopic submucosal dissections (with video). Gastrointestinal Endosc 2007; 66: 966-973.
- González N, Parra-Blanco A, Villa-Gómez M,Gamba A, Taullard A, Silveira A, Sanguinetti A, Olano C, Cohen H. Gastric endoscopic submucosal dissection: From animal model to patient. World J Gastroenterol 2013; 19: 8326-8334.
- Tanimoto MA, Torres-Villalobos G, Fujita R, Santillan-Doherty P, Albores-Saavedra J, Chable-Montero F, Martin-Del-Campo LA, Vasquez L, Bravo-Reyna C, Villanueva O, Villalobos JJ, Uribe M, Valdovinos MA. Learning curve in a Western training center of the circumferential en bloc esophageal endoscopic submucosal dissection in an in vivo animal model. Diagn Ther Endosc 2011; 2011: 847831.
- Tanimoto MA. Submucosal endoscopic dissection. Rev Gastroenterol Mex 2010; 75: 177-185.
- Sugimoto T, Okamoto M, Mitsuno Y, Kondo S, Ogura K, Ohmae T, Mizuno H, Yoshida S, Isomura Y, Yamaji Y, Kawabe T, Omata M, Koike K. Endoscopic submucosal dissection is an effective and safe therapy for early gastric neoplasms: a multicenter feasible study. J Clin Gastroenterol 2012; 46: 124-129.
- Parra-Blanco A, Saito Y, Yahagi N. Recommendations about training for colorectal endoscopic submucosal dissection in the western world. Results of a survey to experts. Gastrointest Endosc 2011; 73: AB419-AB420.
- Kakushima N, Fujishiro M, Kodashima S, Muraki Y, Tateishi A, Omata M. A learning curve for endoscopic submucosal dissection of gastric epithelial neoplasms. Endoscopy 2006; 38: 991-995.
- Choi IJ, Kim CG, Chang HJ, Kim SG, Kook MC, Bae JM. The learning curve for EMR with circumferential mucosal incision in treating intra mucosal gastric neoplasm. Gastrointest Endosc 2005; 62: 860-865.
- Yamamoto S, Uedo N, Ishihara R, Kajimoto N, Ogiyama H, Fukushima Y, Yamamoto S, Takeuchi Y, Higashino K, Iishi H, Tatsuta M. Endoscopic submucosal dissection for early gastric cancer performed by supervised residents: assessment of feasibility and learning curve. Endoscopy 2009; 41: 923-928.
- Yamamoto Y, Fujisaki J, Ishiyama A, Hirasawa T, Igarashi M. Current status of training for endoscopic submucosal dissection for gastric epithelial neoplasm at Cancer Institute Hospital, Japanese Foundation for Cancer Research, a famous Japanese hospital. Dig Endosc 2012; 24: 148-153.
- Dinis-Ribeiro M, Pimentel-Nunes P, Afonso M, Costa N, Lopes C, Moreira-Dias L. A European case series of endoscopic submucosal dissection for gastric superficial lesions. Gastrointest Endosc 2009; 69: 350-355.
- Ohata K, Ito T, Chiba H, Tsuji Y, Matsuhashi N. Effective training system in colorectal endoscopic submucosal dissection. Dig Endosc 2012; 24: 84-89.
- Shiga H, Kuroha M, Endo K, Kimura T, Kakuta Y, Kinouchi Y, Kayaba S, Shimosegawa T. Colorectal endoscopic submucosal dissection (ESD) performed by experienced endoscopists with limited experience in gastric ESD. Eur J Gastroenterol Hepatol 2014; 26: 949-954.
Correspondencia: Nicolás González
Av Italia 2870 – Piso 4. Montevideo 11600, Uruguay
Fax: +598-2-4808472
Correo electrónico: nicolasendoscopia@yahoo.es
Acta Gastroenterol Latinoam 2016;46(3): 213-219
 Revista ACTA Órgano Oficial de SAGE
Revista ACTA Órgano Oficial de SAGE