Lina Paola Tovar1 ID· Jean Paul Gómez2 ID· Adriana Margarita Trejos3 ID
1 Hospital Universitario San Vicente Fundación. Medellín, Colombia
2 Universidad de Antioquia
3 Universidad Pontificia Bolivariana
Acta Gastroenterol Latinoam 2021;51(4):446-449
Received: 01/09/2021 / Accepted: 15/11/2021 / Published in www.actagastro.org 13/12/2021 / https://doi.org/10.52787/XEYK2378
Summary
Entamoeba histolytica infection is common in developing countries such as Colombia. Its clinical presentation is variable and not very specific. Within this variety, ameboma is arare manifestation characterized by tumor growth secondary to the formation of granulation tissue in the colonic walls. This growth can be indistinguishable from a neoplasm, so a high index of clinical and endoscopic suspicion must be present to make an adequate diagnostic and therapeutic approach. We present the case of a patient with amebiasis, whose symptoms and imaging presentation were mistaken for colon carcinoma with liver metastases.
Keywords. Entamoeba histolytica, ameboma, amebic liver abscess, colorectal carcinoma.
Ameboma rectal y abscesos hepáticos: un simulador de cáncer colorrectal
Resumen
La infección por Entamoeba histolytica es común en países en desarrollo como Colombia. Su presentación clínica es variable y poco específica. Dentro de esta variedad, el ameboma es una manifestación infrecuente, y se caracteriza por un crecimiento tumoral secundario a la formación de tejido de granulación en las paredes colónicas. Ese crecimiento puede ser indistinguible de una neoplasia, por lo que se debe tener un alto índice de sospecha clínica y endoscópica para realizar el abordaje diagnóstico y terapéutico adecuado. Presentamos el caso de un paciente con amebiasis, cuyos síntomas y presentación imagenológica fueron confundidos con un carcinoma de colon con metástasis hepáticas.
Palabras claves. Entamoeba histolytica, ameboma, absceso hepático amebiano, carcinoma colorectal.
Introduction
Amebiasis, caused by Entamoeba histolytica, is one of the most frequent parasitosis diseases, with an estimated 34 to 50 million symptomatic cases and 100,000 deaths per year worldwide, and the highest burden of morbidity and mortality in Central and South America, Africa and India.1 It is an endemic condition in countries with poor sanitation services. However, only 10% of the infected population will develop symptoms.1
Clinical presentation is variable, ranging from diarrhea with or without dysentery to infrequent complications such as toxic megacolon or perianal ulceration.2 Extraintestinal manifestations can occur, the most frequent of which is liver abscess, typically described as single and localized in the right lobe in 80% of cases.2 It is estimated that only 1.5% of patients will manifest an ameboma, a chronic complication characterized by a concentric colonic mass that can obstruct the lumen and generate obstructive symptoms.3
The coexistence of ameboma and liver abscesses is uncommon3, hence the macroscopic and imaging appearance of these lesions can be confused with metastatic colon carcinoma.
Case Report
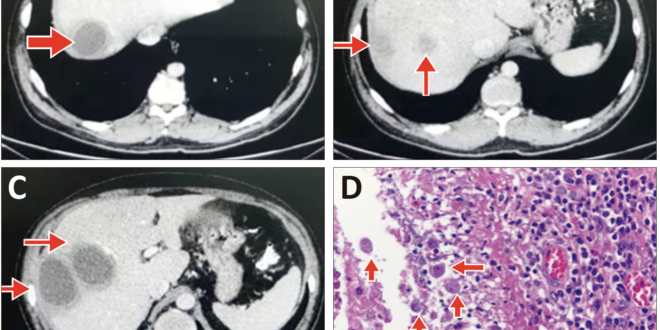
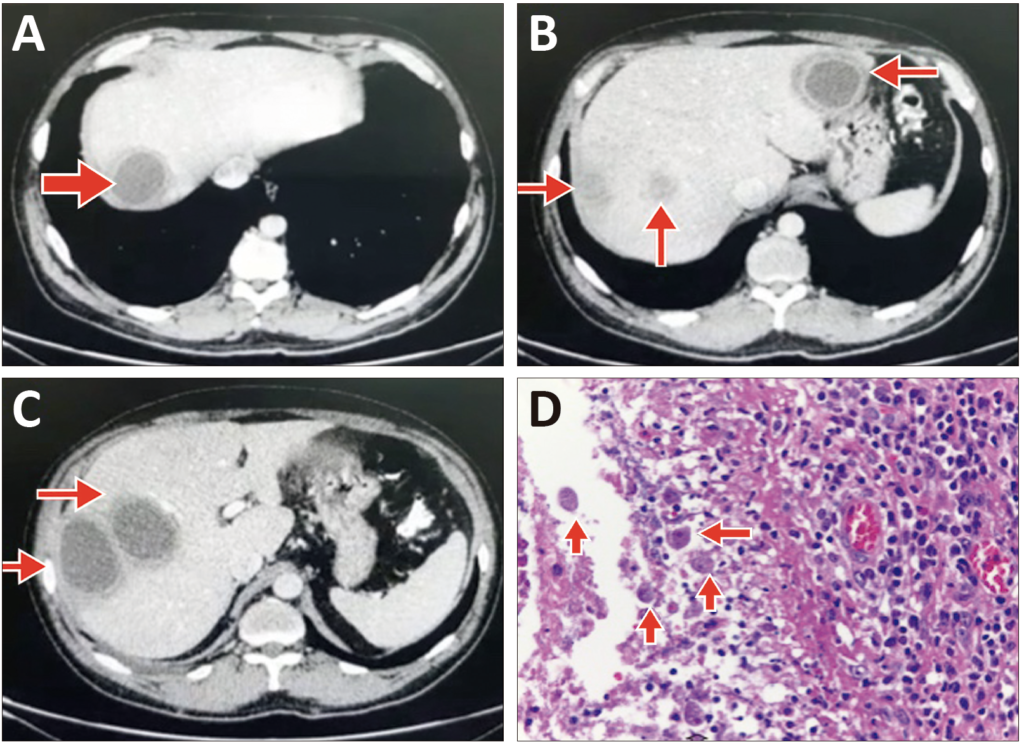
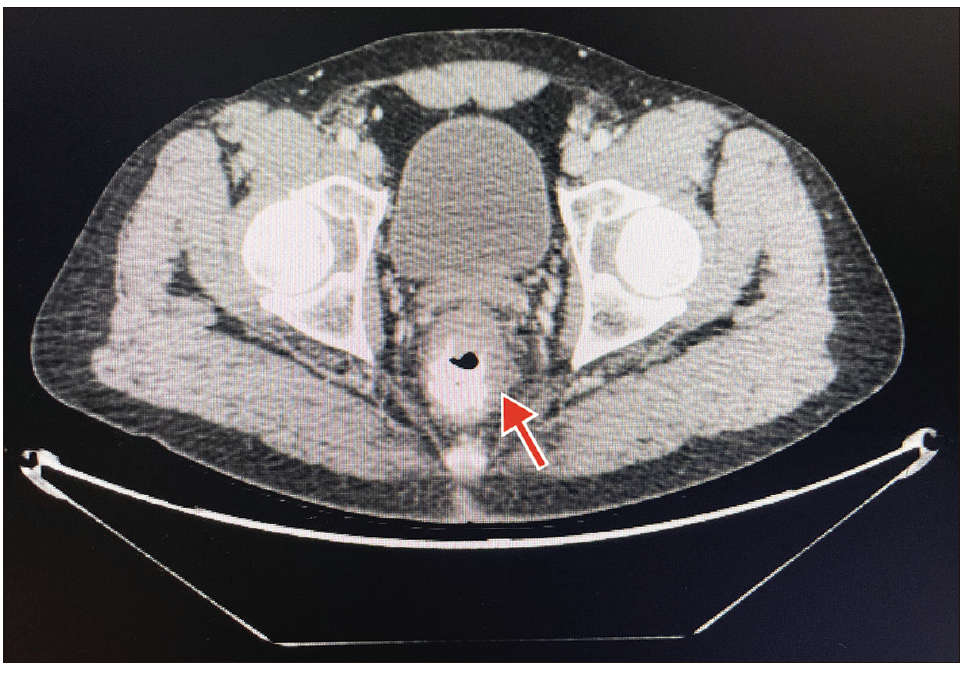
A 44-year-old man, with a history of heavy smoking and unexplained weight loss of 10 kg in the last month, consulted for a one-day clinical picture of generalized abdominal pain and nausea. Laboratory studies reported leukocytosis (12,000 cell/mm3) with neutrophilia (60%) and eosinophilia (6%), normal liver and kidney function, and negative HIV serology. An initial abdominal ultrasound showed multiple liver lesions with cystic and solid content, the largest (34×32 mm) located in the segment VII of the right hepatic lobe. Subsequently, a contrasted abdominal CT scan was performed (Figure 1 A, B, C), which confirmed four hypodense liver lesions of low attenuation and slight enhancement, ranging between 5.3 cm and 6.1 cm in diameter, with irregular thickening of the rectum with an approximate extension of 6 cm (Figure 2). Total colonoscopy confirmed the presence of an ulcerated lesion with fibrin and granulation tissue, of approximately 5 cm x 2 cm, occupying 30% of the circumference of the rectum, from which the respective biopsies were taken. The patient was evaluated by oncology and general surgery, who considered a high probability of metastatic carcinoma of the rectum, metastatic to the liver. The iniation of chemotherapy was planned.
Figure 1. Computed tomography (CT) with abdominal contrast and tissue biopsy of the colonic mass. Low attenuation lesions (red arrows) and peripheral enhancement with contrast located in the right hepatic lobe (A and C) (segments, V, VI, VII, mean diameter 53 mm) and left hepatic lobe (B) (between segment II and II of 61 mm in diameter). Periodic Acid-Schiff (PAS) staining demonstrates the presence of abundant protozoal structures (red arrows), compatible with Entamoeba histolytica (D).
Figure 2. Computed tomography (CT) with abdominal contrast. Irregular thickening of the lower and middle rectum, extension of approximately 6 cm with dominant irregularity of 2 cm in the internal wall. Increased attenuation and nodularity of perirectal fat.
Prior to chemotherapy, a histopathology report of the rectal mucosa was received, with a description of severe chronic active ulcerative inflammation associated with ameba trophozoites (Figure 1D). With the diagnosis of rectal ameboma and liver abscesses, treatment was started with 500 mg of intravenous metronidazole every eight hours for 14 days and teclozan 500 mg orally every 12 hours for five days, in addition to percutaneous drainage of liver lesions, from which approximately 50 cc of purulent material was obtained. Microbiological studies of the purulent material corresponding to direct stains (microscopic search for amebiasis, gram, Ziehl Neelsen, KOH), polymerase chain reaction for tuberculosis, cultures for aerobes, mycobacteria and fungi were negative. The patient was discharged, after five days of hospitalization, with a complete improvement of symptoms and liver lesions on ultrasound control.
Discussion
Amebiasis is an important parasitic disease worldwide, especially in tropical regions. Although it predominantly affects the colon, the liver is the most frequent extraintestinal involved location.4 Unusually, patients with chronic or partially treated infection develop exophytic inflammatory masses known as amebomas.5 These tumors predominate in men between 20 and 60 years of age and their most frequent anatomical involvement is rectosigmoid, as in our patient. Symptoms are nonspecific, including abdominal pain, diarrhea and constipation, as well as weight loss and fever. Its most common differential diagnosis is colorectal carcinoma, but it can also be confused with diverticular disease and Crohn’s disease.6
Conventional diagnostic methods for amebiasis, such as stool microscopy, can help if trophozoites or cysts are seen; however, their sensitivity is low, being 60% at best for amebic colitis. Performing colonoscopy plus a biopsy of the visualized lesions, together with a high suspicion on the part of the endoscopist, can facilitate the diagnosis and identification of amebomas, using Periodic Acid-Schiff (PAS) stains.4,7
The main treatment for both colitis and amebic liver abscess are nitroimidazoles, with metronidazole being the most widely used. Since parasites can persist in the intestinal lumen in up to 40% of patients treated with tissue agents, treatment with nitroimidazoles must be accompanied by luminal agents, such as teclozan.4
Percutaneous drainage of abscesses is occasionally necessary in patients with poor response to initial medical treatment or in those at risk of rupture, for example, a diameter greater than 5 cm or located in the left lobe. In the case of the reported patient,, it was decided to perform drainage early, both due to size and location.
Ameboma in association with liver abscesses is a rare condition. Among the reported cases,3,5,6,8,9 the elements common to ours were the predominant presentation in middle-aged men (between 40 and 60 years) who consulted due to acute symptoms of abdominal pain, fever, and changes in bowel habits (diarrhea or constipation).
Perhaps the most important point to note is that in all the above cases the diagnosis was made postoperatively, with a histological study of the samples taken in surgery. This finding is due to an urgent surgical indication for intestinal obstruction3,5,9 or to a management consistent with a high suspicion of malignancy despite negative biopsies at colonoscopy.6
It should also be taken into account that, in the previously reported cases,5,6,8 the size of the liver lesions was smaller and none required drainage; additionally, imaging controls, performed between four to eight weeks after receiving antiparasitic treatment, showed that the liver lesions had been completely resolved.
Conclusion
In conclusion, we consider that amebiasis, as a frequent entity, especially in developing countries, should be included in the differential diagnoses of acute abdomen with colon mass. A high index of suspicion is required in the diagnostic process of these patients to avoid unnecessary treatments and surgery.
Key Points
- Amebiasis is a frequent entity, especially in developing countries
- The unusual presentation, called ameboma, should be included in the differential diagnoses of acute abdomen with colon mass.
- A high index of suspicion is required in the diagnostic process of these patients to avoid unnecessary treatments and surgeries.
Conflict of interest. None of the authors has a conflict of interest related to the manuscript.
Consent for Publication. Written informed consent was obtained from the patient or their parent, guardian, or relative to publish the data and/or clinical images for the benefit of science. A copy of the consent form is available to the editors of this journal.
Intellectual Property. The authors declare that the data and figures that appear in this article are original and were made in their belonging institutions.
Copyright
 © 2021 Acta Gastroenterológica latinoamericana. This is an open-access article released under the terms of the Creative Commons Attribution (CC BY-NC-SA 4.0) license, which allows non-commercial use, distribution, and reproduction, provided the original author and source are acknowledged.
© 2021 Acta Gastroenterológica latinoamericana. This is an open-access article released under the terms of the Creative Commons Attribution (CC BY-NC-SA 4.0) license, which allows non-commercial use, distribution, and reproduction, provided the original author and source are acknowledged.
Cite this article as: Tovar P L, Gomez J P, Trejos A M. Rectal Ameboma and Liver Abscesses: A Colorectal Cancer Simulator. Acta Gastroenterol Latinoam. 2021;51(4):446-9. https://doi.org/10.52787/XEYK2378
References
- Bercu TE, Petri WA, Behm BW. Amebic colitis: New insights into pathogenesis and treatment. Curr Gastroenterol Rep. 2007;9(5):429–33.
- Haque R, Huston C. Amebiasis: Review Article. N Engl J Med. 2003;348(16):1565–73.
- Li Peng T, Kee KF, Lim Yal. A colonic amoebic abscess mimicking colonic carcinoma. Med J Malaysia. 2018;73(5):334–5.
- Petri WA, Haque R. Entamoeba Species, Including Amebic Colitis and Liver Abscess [Internet]. Ninth Edit. Vol. 2, Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Elsevier Inc.; 2020. 3047-058.e1 p. Available from: https://doi. org/10.1016/B978-0-323-48255-4.00272-1
- Moorchung N, Singh V, Srinivas V, Jaiswal S, Singh G. Caecal amebic colitis mimicking obstructing right sided colonic carcinoma with liver metastases: A rare case. J Cancer Res Ther. 2014;10(2):440–2.
- Fernandes H, D’Souza CR, Swethadri GK NC. Ameboma of the colon with amebic liver abscess mimicking metastatic colon cancer. J Pathol Microbiol. 2009;52(2):228-230.
- Abe T, Kawai N, Yasumaru M, Mizutani M, Akamatsu H, Fujita S, et al. Ameboma mimicking colon cancer. Gastrointest Endosc [Internet]. 2009;69(3 SUPPL.):757–8. Available from: http://dx.doi.org/10.1016/j.gie.2008.12.065
- Ng DCK, Kwok SY, Cheng Y, Chung CC, Li MKW. Colonic amoebic abscess mimicking carcinoma of the colon. Hong Kong Med J. 2006;12(1):71–3.
- Radovanovic ZL, Katic V V., Nagorni A V., Zivkovic V V., Stankovic TD, Trenkic MS. Clinical diagnostic problems associated with cecal ameboma. Case report and review of the literature. Pathol Res Pract. 2007;203(11):823–5.
Correspondence: Lina PaolaTovar
Email: linaptovar@hotmail.com
Acta Gastroenterol Latinoam 2021;51(4):446-449
 Revista ACTA Órgano Oficial de SAGE
Revista ACTA Órgano Oficial de SAGE