Eudaldo López Tomassetti Fernández, David Fernández-San Millán, Juan Ramón Hernández Hernández
Department of Gastrointestinal Surgery, Complejo Hospitalario Insular de Gran Canaria (CHUIMI). Spain.
Acta Gastroenterol Latinoam 2017;47(3):225-229
Recibido: 05/02/2017 / Aprobado: 01/06/2017 / Publicado en www.actagastro.org el 02/10/2017
Summary
A 32 year-old patient with a BMI of 63 kg/m2 underwent laparoscopic Scopinaro biliopancreatic diversion at our hospital in September 2014 (alimentary limb measuring 250 cm and common channel 65 cm). His postoperative course was uneventful and was discharged home on a clear liquid diet at fourth postoperative day, free of drains and with proper instructions provided regarding vitamins, mineral supplementation and one month course of low-molecular-weight heparin. One month after surgery he complained of vomits and acute abdominal distention. CT-scan of the abdomen was done showing a moderately distended stomach and ileal short segment stricture in close proximity to the gastroileal anastomosis. Results. This case report describe clinical, endoscopic and radiologic findings in a patient who developed acute abdominal distension and vomiting, secondary to short segment ileal affection by Crohn disease (CD). We also discussed why patient could have had excellent response to medical treatment. Aminosalicylates inhibit the proinflammatory factor NFkappa Beta. Sulfasalazine and 5-ASA inhibit new prostaglandin synthesis, free radicals activity of lymphocytes, monocytes and other proinflammatory cytokines such as interleukin 1 or TNF-alpha. In those patients with only small bowel involvement mesalamine could be the treatment of choice. Conclusions. Disturbances in hormonal function of adipose tissue in obesity seem to modulate immune activity and participate in the pathogenesis as well as the course of IBD.
Key words. Adipokines, biliopancreatic diversion, Crohn disease, ileal diseases, mesalamine, overweight.
Obstrucción aguda del asa alimentaria como debut de enfermedad de Crohn
Resumen
Un paciente de 32 años con un IMC de 63 kg/m2 fue sometido a una derivación laparoscópica biliopancreática de Scopinaro en nuestro hospital en septiembre de 2014 (asa alimentaria de 250 cm y canal común de 65 cm). Su postoperatorio discurrió sin incidentes y fue dado de alta domiciliaria con una dieta líquida clara en el cuarto día del postoperatorio, libre de drenajes y con las instrucciones adecuadas sobre vitaminas, suplementos minerales y un mes de tratamiento con heparina de bajo peso molecular. Un mes después de la cirugía se quejó de vómitos y distensión abdominal aguda. Se realizó una tomografía axial computarizada del abdomen mostrando una estenosis del estómago moderadamente distendido y del segmento corto ileal en proximidad cercana a la anastomosis gastroileal. Resultados. Este caso describe hallazgos clínicos, endoscópicos y radiológicos en un paciente que desarrolló distensión abdominal aguda y vómitos secundarios a una afección ileal del segmento corto por enfermedad de Crohn. También discutimos por qué el paciente pudo haber tenido una excelente respuesta al tratamiento médico. Los aminosalicilatos inhiben el factor proinflama torio NFkappa Beta. La sulfasalazina y el 5-ASA inhiben la nueva síntesis de prostaglandinas, la actividad de los radicales libres de los linfocitos, los monocitos y otras citoquinas proinflamatorias como la interleucina 1 o el TNF-alfa. En los pacientes con sólo la participación de intestino delgado, la mezalamina podría ser el tratamiento de elección. Conclusiones. Los trastornos en la función hormonal del tejido adiposo en la obesidad parecen modular la actividad inmune y participar en la patogénesis, así como en el curso de la EII.
Palabras claves. Adipokinas, derivación bilipancreática, enfermedad de Crohn, enfermedad ileal, mesalazina, sobrepeso.
A 32 year-old patient with a BMI of 63 kg/m2 underwent laparoscopic Scopinaro biliopancreatic diversion at our hospital in September 2014 (alimentary limb measuring 250 cm and common channel 65 cm). His postoperative course was uneventful and was discharged home on a clear liquid diet at fourth postoperative day, free of drains and with proper instructions provided regarding vitamins, mineral supplementation and one month course of low-molecular-weight heparin.
One month after surgery he complained of vomits and acute abdominal distention. CT-scan of the abdomen was done showing a moderately distended stomach and ileal short segment stricture in close proximity to the gastroileal anastomosis.
This case report describe clinical, endoscopic and radiologic findings in a patient who developed acute abdominal distension and vomiting secondary to short segment ileal affection by Crohn disease (CD). We also discussed why patient could have had excellent response to medical treatment.
Case report
A 32 years old male patient was admitted to our hospital on September 2014 for abdominal distention with vomiting. He also complained of difficulty in passing stools. He had no history of abdominal trauma or any other systemic complaints and had undergone laparoscopic Scopinaro BPD one month ago. On examination, his BMI was 58 kg/m2 and his vitals were within normal limits. Blood, urine and biochemical tests (including serum pancreatic amylase and lipase) were unremarkable.
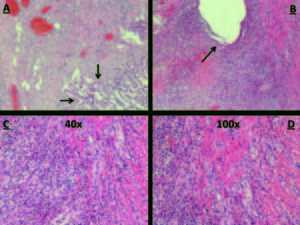
Abdominal film suggested gastric dilatation and CT-scan (Figure 1) showed gastric dilatation to the level of the gastroileal anastomosis and short segment of ileal wall thickening in close proximity to the anastomosis. Nasogastric tube was inserted to aspirate stomach contents and to decompress it. Upper endoscopy (Figure 2) showed a 5 to 40 cm inflamed segment of ileum just distal to the anastomosis, which showed ulcerative lesions with ring structures resembling CD. Gastroileal anastomosis was normal and stenosis was not observed. Stenosed segment was balloon dilated up to 20 mm and biopsy was carried out. Surprisingly, pathological study confirmed active ileal CD with mild to moderate chronic active inflammation, some ulcerations and inflammatory granulation tissue from a site of deep ulceration (Figure 3).
Figura 1. Gastric dilatation to the level of gastro-ileal anastomosis.
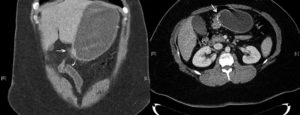
Figura 2. Ulcerative lesions with ring structures resembling Corhn´s disease.
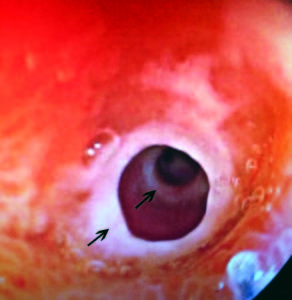
Figura 3. A) Inflammation of the lamina propria and distortion of intestinal crypts. B) Intestinal fissure. C) Pseudogranuloma x40. D) Pseudogranuloma x100.
Intravenous steroids (urbason 80 mg/day) were administered immediately after endoscopy and patient started liquid diet on the fourth day after admission. He was discharged home without any complaint at sixth day with soft diet, oral budesonide 9 mg/day for two weeks, mesalazine 1.000 mg orally daily, and sequential balloon dilation scheduled at two weeks and one month after the first session. Three months after treatment, upper endoscopy showed complete resolution of the ileal disease and mesalazine was discontinued without new relapse at two years follow-up.
Discussion
Inflammatory bowel disease is considered to be a disease that mainly affects young people. It presents a bimodal distribution with two peaks of age affecting also in the 5th-8th decades. Environmental factors such as solar exposure, infectious agents, or physical activity can determine the evolution of the CD. Some studies have shown an increase in carbohydrate intake in these patients and the effect of refined sugars, fish, vegetables, fruit, margarine and coffee consumption among others has been studied.
Obesity has been increasingly prevalent over the world and recent literature highlights significant association between CD and obesity.1 In fact, excess fat mass has been associated with immune dysregulation resulting in a continuous proinflammatory state and it is also linked with markers of increased intestinal permeability that may facilitate translocation of intestinal bacteria.1 Cytokines such as interleukin-6 or TNF-alpha are overexpressed and adipokines like leptin, adiponectin and resistin are also produced within adipocytes in the mesenteric fat inducing a proinflammatory profile in obesity. Adipokines are critical mediators that convey information about adipose tissue status to the body. Obese subjects produce high levels of leptin but are resistant to its activity. Leptin is a survival and activating factor for T lymphocytes and promotes proinflammatory responses. Adiponectin has antiinflammatory effects and its levels are reduced in obesity. However, levels of adiponectin are paradoxically elevated and positively associated with markers of inflammation in chronic inflammatory diseases.
High-molecular-weight adiponectin seem to be the most active and proinflammatory isoforms. Salani et al, demonstrated that this adiponectin increase their levels one month after a bilio-pancreatric diversion. The influence of the weight loss on this adiponectin is unknown. It could be due to the activation of the proliferator receptor of peroxisoms that occurs when there is a negative energy balance.2
Recent study in Brazil, evaluated 64 patients with CD and overweight was diagnosed in 37.5% of patients. In this study, use of steroids and immunosuppressive drugs were not associated with overweight.3 In Ireland, a prospective study was conducted in comprising 100 CD outpatients and 100 matched healthy controls, 40% of CD patients were overweight or obese. They reported that, overweight was common in outpatients with CD and appeared to reflect current wellness, older age and sedentary lifestyles.4 However, prevalence rate of overweight and obesity among CD patients is very low in Japan. As the author suggest, rise in the incidence of CD has paralleled the social and economic development of populations and adaptation to Western lifestyles including diet changes. However, in Japan this difference may be due to the difference in genetic background.5 For example, overexpression of recently discovered CARD15/Nod2 gene in Caucasians could explain this difference. NOD2 gene encodes a protein that activates NF – kappa Beta sensitive to certain bacterial lipopolysaccharide factor. Patients with overexpression of this gene could respond inappropriately to certain intestinal bacteria developing chronic bowel inflammation. Taken together, these data suggest that obesity itself may be a risk factor for the development of inflammatory bowel disease.
Interestingly, there are some recent reports concerning potential association between CD and bariatric surgery.6, 7 Hypothesis suggest that bacterial overgrowth can develop as a consequence of the altered anatomy after surgery in gastric bypass and this anatomic changes may promote a bacterial milieu in genetically predisposed patients that triggers chronic intestinal inflammation, resulting in CD. Petrolesi published a similar case to ours in which it was affected the biliopancreatic limb.8 Our case is the first description of a patient with biliopancreatic diversion with obstruction of the alimentary limb from CD and our hypothesis suggest that rise of serum proinflammatory high-molecular-weight adiponectin may also have been involved as demonstrated by Salani, because bacterial overgrowth is uncommon in the first month after surgery.
On the other side, there are several reports in the literature addressing the outcome of CD activity and obesity surgery. While the case presented by Lascano et al seems to demonstrate some degree of improved disease activity after obesity surgery in ulcerative colitis, this promising observation needs further validation.9 Ahn et al reported three morbidly patients that underwent a Roux-en-Y gastric bypass and developed newly diagnosed CD within 11–60 months of surgery.6 They were all young adults (28–46 years old), who presented with watery diarrhea, nocturnal diarrhea accompanied by abdominal cramps and more than expected weight loss. Endoscopic evaluation revealed ulcers with histological features pathognomonic for CD. All patients responded to medical management and are well with at least one year follow-up. Moun et al presented a case of a 40 year old woman with ileocolic CD medically controlled with infliximab for four years, who had a BMI of 45 kg/m2, type II diabetes and hypertension.10 The patient underwent a Roux-en-Y gastric bypass, and eight weeks postoperatively she had gradually increasing abdominal pain and diarrhea. Endoscopy revealed active ileocolic CD. She underwent high dose infliximab therapy, which controlled her symptoms and eight months postoperatively, she was still in disease remission.
Results
Aminosalicylates inhibit the proinflammatory factor NFkappa Beta. Sulfasalazine and 5-ASA inhibit new prostaglandin synthesis, free radicals activity of lymphocytes, monocytes and other proinflammatory cytokines such as interleukin 1 or TNF-alpha. In those patients with only small bowel involvement mesalamine could be the treatment of choice. Recent studies have also shown that, 4 gr of mesalamine on a daily basis are as effective as 40 mg/day of methylprednisolone for treating an active ileitis in the context of CD.11
In biliopancreatic diversion, gastric pouch is anastomosed to an ileal segment (gastroileal anastomosis) completely bypassing the upper part of the small intestines. A common channel remains in which, bile and pancreatic digestive juices mix prior to entering the colon. We believe that, our patient had a surprising response due to the fact that mesalazine acts more quickly, with less degradation of the active metabolite and, therefore, with greater efficiency topically in the mucosa due to the bypass of the duodenum and yeyunum.
In our case, CD was diagnosed 5 weeks after surgery; therefore we suspected that our patient could have had CD before surgery with an isolated asymptomatic ileitis. Before surgery, he had normal abdominal ultrasound, upper endoscopy without helicobacter pylori and normal blood test without raised inflammatory markers such as CRP. Moreover, macroscopic signs of CD such as fat wrapping of the ileum were not noticed by the surgical team and patient had never complained for symptoms suggestive of inflammatory bowel disease. Differentiation between CD and an ischemic gastroileal anastomosis was critical to develop a treatment plan. Gastroileal antecolic anastomosis was tension-free which discards an ischemic ileal segment as a possible cause for stenosis. In addition, gastroileal anastomosis was non-stenotic and involvement of a 60 cm discontinuous segment of proximal ileum with patchy involvement excluded an ischemic etiology.
Conclusion
Our patient lost 80 kg a year postoperatively and CD definitively improved with mesalazine in a similar way to reported cases.6, 9, 10 Three months after surgery, coinciding with the loss of weight, he discontinued oral mesalazine without further relapses at two years follow-up. We think that, disturbances in hormonal function of adipose tissue in obesity seem to modulate immune activity and participate in the pathogenesis as well as the course of IBD. Undoubtedly, this theory requires more information and further studies. Excellent response and remission with oral mesalazine was reported by us; however, we do not know whether this improvement was due to medical treatment or improvement of chronic inflammation associated with weight loss.
Conflict of interest. None.
Author contributions. All authors contributed equally.
Funding. No specific funding has been received; data have been generated as part of the routine work of the Complejo Hospitalario Insular de Gran Canaria.
Referencias
- Moreno-Navarrete JM, Sabater M, Ortega F, Ricart W, Fernández- Real JM. Circulating zonulin, a marker of intestinal permeability, is increased in association with obesity-associated insulin resistance. PLoS One. 2012; 7: e37160.
- Salani B, Briatore L, Andraghetti G, Adami GF, Maggi D, Cordera R. High-molecular weight adiponectin isoforms increase after biliopancreatic diversion in obese subjects. Obesity 2006; 14: 1511-1514.
- Nascimento AT, Rocha R, Coqueiro FG, Santana GO, Lyra AC. Does obesity complicate inflammatory bowel disease? J Crohns Colitis 2012; 6: 1041.
- Nic Suibhne T, Raftery TC, McMahon O, Walsh C, O’Morain C, O’Sullivan M. High prevalence of overweight and obesity in adults with Crohn’s disease: associations with disease and lifestyle factors. J Crohns Colitis 2013; 7: e241-e248.
- Yamamoto T, Shiraki M. Prevalence of overweight and obesity in patients with Crohn’s disease in Western countries and Japan. J Crohns Colitis 2013; 7: e192.
- Ahn LB, Huang CS, Forse RA, Hess DT, Andrews C, Farraye F. Crohn’s disease after gastric bypass surgery for morbid obesity: Is there an association? Inflamm Bowel Dis 2005; 11: 622-624.
- Janczewska I, Nekzada Q, Kapraali M. Crohn’s disease after gastric bypass surgery. BMJ Case Rep 2011; 2011: 2010-2012.
- Pretolesi F, Camerini G, Marinari GM, Stabilini C, Capaccio E. Crohn disease obstruction of the biliopancreatic limb in a patient operated for biliopancreatic diversion for morbid obesity. Emerg Radiol 2006; 12: 116-118.
- Lascano CA, Soto F, Carrodeguas L, Szomstein S, Rosenthal RJ, Wexner SD. Management of ulcerative colitis in the morbidly obese patient: Is bariatric surgery indicated? Obes Surg 2006; 16: 783-786.
- Jahnsen BMJ. Bariatric surgery in inflammatory bowel disease. Tidsskr Nor Laegeforen 2010; 130: 638-689.
- Healey JN. Gastrointestinal transit and release of mesalazine tablets in patients with inflammatory bowel disease. Scand J Gastroenterol 1990; 172: 47-51.
Correspondencia: David Fernández San Millán
Dirección: Avda. Marítima s/n 35016, Las Palmas de Gran Canaria, Canary Islands, Spain.
Tel: +34 636977787
Correo electrónico: san_millan@hotmail.com
Acta Gastroenterol Latinoam 2017;47(3): 225-229
 Revista ACTA Órgano Oficial de SAGE
Revista ACTA Órgano Oficial de SAGE


