Rikki Singal,1 Shyam Trehan,1 Amit Mittal,2 Maitrayee Roy,3 Kusum Joshi3
1 Department of Surgery.
2 Department of Radiology.
3 Department of Pathology.
Maharishi Markandeshwer Institute of Medical Sciences and Research. Mullana, Distt-Ambala, Haryana, India.
Acta Gastroenterol Latinoam 2018;48(1):52-55
Recibido: 16/01/2017 / Aprobado: 22/11/2017 / Publicado en www.actagastro.org el 19/03/2018
Summary
Retroperitoneal liposarcoma (RL) is a relatively rare tumour and is usually found at the advanced stage. Liposarcoma are one of the common soft tissue tumors of adulthood which are remarkable because of their frequently large size. We report a case presented as huge mass and diagnosed as differentiated retroperitoneal liposarcoma that weighted 40 Kilograms. Complete resection of tumour with wide margins including excision of other organs has been recommended.
Key words. Liposarcoma, bowel loops, retroperitoneal, kidney, ureter, soft tissue tumour.
Sarcoma retroperitoneal gigante: patología actual y éxito quirúrgico
Resumen
El liposarcoma retroperitoneal (LR) es un tumor relativamente raro y generalmente se diagnostica en estadio avanzado. Es uno de los tumores de tejidos blandos más comunes de la edad adulta, y son notables debido a su tamaño frecuentemente grande. Presentamos un caso de LR como una masa enorme de 40 kilogramos. Recomendamos la resección completa del tumor con márgenes amplios, incluida la extirpación de otros órganos.
Palabras claves. Liposarcoma, asas intestinales, retroperitoneal, riñón, uréter, tumor de tejidos blandos.
Retroperitoneal sarcomas are rare tumors, having an annual incidence of 0.3 to 0.4 new cases per 100.000 habitants.1 Liposarcoma is a rare type of malignant tumour, that arises in fat cells in deep soft tissue.2 The liposarcoma may have weight and dimension variable; those over 20 kg are called “giant liposarcomas” and are extremely rare.3 Patient usually occurs symptoms of pain or functional disturbances only when the tumour is very large. Well-differentiated liposarcomas treated with surgery and radiations have a low recurrence rate (about 10%) and rarely metastasize. Five-year survival rates vary from 100% to 56% based on histological subtype.4
Case report
We present a case of 55 years old Indian male, who presented in our OPD with an abdominal swelling since 15 days. It was seen more in left lumbar area which increased in size progressively and occupied most of the abdominal cavity. Patient also gives a history of low grade intermittent fever without any loss of appetite during these 15 days. The patient was having no significant history associated with swelling. On examination, no abnormal finding was seen, and local examination revealed a huge swelling of size 20 x 20 cm occupying whole of left lumbar area extending upto left iliac fossa and crossing the midline. The lump felt was firm to hard in consistency, non-tender, temperature not raised and not moving with respiration. There were no visible pulsations or movements. Patient underwent routine investigations which were within normal limits.
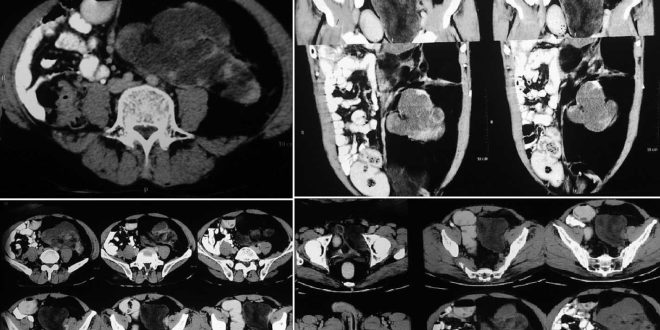
Ultrasonography (USG) revealed a large mixed echogenicity lesion in the left lumbar, umbilical and hypogastric area with hypoechoic solid areas. Contrast enhanced computed tomography (CECT) of abdomen shows a huge heterogeneously enhancing mass approx 28 × 12 × 9.3 cm in retroperitoneum on left side involving the anterior pararenal space displacing colon anteriorly (Figure 1). Mass is extending into perirenal space abutting the renal cortex. Solid component showing low density areas are seen within the mass. It is crossing to midline anterior to aorta. After undergoing all the relevant investigations, patient was declared fit for surgery and was taken for laparotomy, a midline incision was made and the findings revealed were as follows (Figure 2):
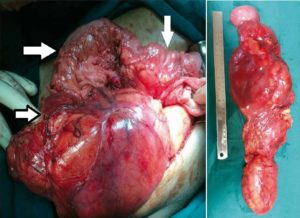
- A huge mass approx 30 × 20 × 10 cm with variegated consistency present in left retroperitoneal space extending from lower pole of left kidney upto pelvic floor, and crossing the midline.
- Mass was densely adherent to left gerotas fascia and mesentery of small bowel.
- Mass was displacing small and large gut towards right side.
- Multiple enlarged lymph nodes and fat lobules present in mesentery of small bowel.
- It was adherent to ureter but not involved it.
- It was removed as encapsulated, lobulated appearance and covered with fibro fatty tissues at some places. On cut section it was identified as firm, variegated appearance, yellowish and myxoid homogeneous.
Figure 1. Computed tomography of the abdomen revealed a huge tumour compressing the bowel loops and extending to the renal area.
Figure 2. A) operative area showing a large tumour (white arrow revealed preserved bowel; black borders arrow reveled tumor), B) resected specimen reveled a huge tumour.
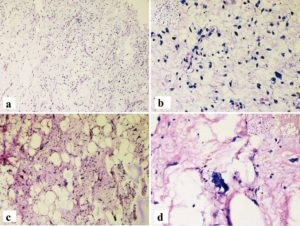
Meticulous dissection was done, and mass was freed from adhesions and removed into including the gerotas fascia. Bowel was saved by blunt dissection of the tumour. Abdomen was closed in layers. On histopathology, it shows multilobulated tumour composed of variable sized adipocytes with presence of scattered lipoblast, floret cells separated by cellular septa. Bizarre lipoblast was seen. Tumour exhibiting abundant hypocellular myxoid area with delicate branching capillary network. Final diagnosis made was myxoid liposarcoma (Figure 3).
Figure 3. A and C) myxoid liposarcoma showing branching delicate capillary sized vessels spindle shaped stromal cells in a myxoid background (H&E, 100X); B and D) stroma cell showing hyperchromatic pleomorphic spindled nuclei, bizarre nuclei and presence of lipoblast (H&E, 400X).
Post-operatively, patient remained stable and was started on orals and drain removed on 6th post op day. Wound remained healthy and the period was uneventful till his discharge from the hospital. In follow up, of 9 months patient remained asymptomatic and disease free. After 16-months of surgery patient came back with recurrence, but he refused for further treatment due to family problem.
Discussion
Retroperitoneal tumour frequently arises from fat, loose connective tissue, fascia, muscles, lymphatic tissue or residual embryonic tissue, of which 80% is malignant. Retroperitoneal liposarcoma is the most commonly seen subtype of retroperitoneal tumour, with an incidence of ~2.5 per million individuals.5 It predominantly found at 40 60 years of age, and the ratio between the genders is ~1:1.3 The common histologic type of retroperitoneal sarcoma (RPS) is liposarcoma (47%), followed by leiomyosarcoma (29%).2 The subtypes of liposarcoma based on morphologic features and cytogenetic aberrations are widely accepted. These include well-differentiated, dedifferentiated, myxoid/round cell and pleomorphic, according to the World Health Organization (WHO) classification.6
USG is routinely choice of first tool before proceeding with computed tomography (CT) scan and magnetic resonant imaging (MRI) for its convenience. On a CT scan, retroperitoneal liposarcoma commonly seen as a large encapsulated mass containing variable amounts of fatty and soft tissue components. MRI is essential to check for invasion of the abdominal aorta or inferior vena cava in cases of liposarcoma. Biopsy is not generally recommended due to the probability of tumour seeding.7 Generally, round cell, pleomorphic and dedifferentiated subtypes are regarded as high grade; whilst well-differentiated and myxoid liposarcoma are low grade. In modernisation of pathological anal¬ysis, greater importance has been attached to the subtypes of retroperitoneal liposarcoma. High histological grade is one of the most important negative prognostic factors in patients with retroperitoneal liposarcoma. Well differentiated liposarcomas may recur locally, but the metastatic potential is low, while pleomorphic liposarcoma have high metastatic potential, which may reduce the survival rate.8 Even, with complete resection of the liposarcoma, prognosis remains poor. The 5-year survival rate of well-differentiated retroperitoneal liposarcoma is 83%, while it is 20% for the dedifferentiated tumour subtype.8 The treatment of choice is complete removal of the tumour and any invaded organs without any residue of the liposarcoma or membrane remaining. The 5-year survival rate may increase from 16.7 to 58%, with the complete dissection of retroperitoneal liposarcoma.9
Even after the surgery, the chances of recurrence of RL commonly seen and the rate was reported from 50% to 85%.10 RL recurs in a huge form, but surgery remains the treatment of choice. Although the chance of a margin-negative resection remains low, adequate resection is associated with an improved survival and hence surgery is preferred for recurrent disease. In our case, whole tumour was excised with margins free. Patient was put on radiotherapy. All diagnostic algorithms and other treatment modalities should be managed by a multidisciplinary team at a high-volume centre that focuses on the care of patients with sarcoma. The decision for preoperative therapy – chemotherapy or radiation – should be based on optimizing the patient for surgical resection.11 The use of radiotherapy is still controversial. The slow growing, well-differentiated liposarcomas are relatively radioresistant. Radiotherapy is generally employed in the treatment of incompletely resected tumors, recurrence at primary site, inoperable primary tumors and metastatic disease. They are also non responsive to various combinations of chemotherapy.11, 12 In our case, because of its huge size, no pre operation radiotherapy or chemotherapy were effective, but post op adjuvant therapy might be indicated. The retroperitoneal liposarcoma is a rare disease with a high rate of recurrence as in our case recurrence was seen.
Conclusion
The complete resection of the retroperitoneal tumour is the choice of treatment. The present study reports a case of giant retroperitoneal liposarcoma which is a challenge for the surgeon owing to the anatomical site, and if adherent to the surrounding structures as seen in our case. We managed well with perseveration of the surrounding structures especially colon mesentery, colon, and the ureter.
Conflict of interest. None.
References
- Hazen B, Cocieru A. Giant Retroperitoneal Sarcoma. J Gastrointest Surg 2017; 21: 602-603.
- Feng D, Xu F, Wang M, Gu X, Ma Z. Anesthetic management of a patient with giant retroperitoneal liposarcoma: case report with literature review. Int J Clin Exp Med 2015; 8: 19530-19534.
- Hashimoto Y, Hatakeyama S, Tachiwada T, Yoneyama T, Koie T, Kamimura N, Yanagisawa T, Hakamada K, Chikara Ohyama Ch. Surgical treatment of a giant liposarcoma in a Japanese man. Adv Urol 2010; 2010: 94307.
- Caizzone A, Saladino E, Fleres F, Paviglianiti C, Iaropoli F, Mazzeo C, Cucinotta E, Macrì A. Giant retroperitoneal liposarcoma: case report and review of the literature. Int J Surg Case Rep 2015; 9: 23-26.
- Neuhaus SJ, Barry P, Clark MA, Hayes AJ, Fisher C, Thomas JM. Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg 2005; 92: 246-252.
- Lee HS, Yu JI, Lim DH, Kim SJ. Retroperitoneal liposarcoma: the role of adjuvant radiation therapy and the prognostic factors. Radiat Oncol J 2016; 34: 216-222.
- Chang IY, Herts BR. Retroperitoneal liposarcoma. J Urol 2013; 189: 1093-1094.
- Nijhuis PH, Sars PR, Plaat BE, Molenaar WM, Sluiter WJ, Hoekstra HJ. Clinico pathological data and prognostic factors in completely resected AJCC stage I-III liposarcomas. Ann Surg Oncol 2000; 7: 535-543.
- Lee SY, Goh BK, Teo MC, Chew MH, Chow PKH, Wong WK, Ooi LL, Soo KC. Retroperitoneal liposarcomas: the experience of a tertiary Asian center. World J Surg Oncol 2011; 9: 12.
- Gholami S, Jacobs CD, Kapp DS, Parast LM, Norton JA. The value of surgery for retroperitoneal. Sarcoma 2009; 2009: 605840.
- Mullinax JE, Zager JS, González RJ. Current diagnosis and management of retroperitoneal sarcoma. Cancer Control 2011; 18: 177-187.
- Aji SA, Alhassan SU, Ibrahim SA. Giant Retroperitoneal Liposarcoma Mimicking Ovarian Tumour – A case report. J West Afr Coll Surg 2011; 1: 105-111.
Correspondencia: Rikki Singal
C/o Dr Kundan Lal Hospital, Ahmedgarh, Distt-Sangrur, Punjab, India. Pin-code: 148021. Tel. celular: 9996184795
Correo electrónico: singalsurgery@yahoo.com
Acta Gastroenterol Latinoam 2018;48(1): 52-55
 Revista ACTA Órgano Oficial de SAGE
Revista ACTA Órgano Oficial de SAGE