Mariano Palermo, Mario Luis Domínguez, Pablo Acquafresca, Guillermo Duza, Mariano Giménez
Department of Gastrointestinal Surgery, Fundación DAICIM and DIAGNOMED, affiliated institution to the University of Buenos Aires, Ciudad Autónoma de Buenos Aires, Argentina.
Acta Gastroenterol Latinoam 2015;45:280-287
Recibido: 22/12/2013 / Aprobado: 24/08/2015 / Publicado en www.actagastro.org el 30/12/2015
Summary
Introduction. Since the first classic descriptions of sur¬gical gastrostomies for feeding by supra-umbilical medial incisions, patients were operated under general anesthesia, with prolonged time of surgery; these were patients in poor health status, undernourished due to inadequate intake or to neurological or tumor involvement, with prolonged hos¬pitalization, both for the recovery of the intestinal motility as well as for the recovery of post-surgical wounds. Therefore, we describe a new minimally invasive technique as an al¬ternative to the percutaneous or endoscopic gastrostomy, in patients where we are not allowed to place a nasogastric tube to insufflate the stomach. This is mostly seen in patients with tumors, which cause obstruction. Material and methods. Between July 2012 and June 2013, 8 patients underwent a single port laparoscopic gastrostomy. Five were females, mean age: 77 years (range: 67-87). In all the patients, it was impossible to place a nasogastric tube, due to obstruc¬tive tumor. Results. The mean time of the procedure was 45 minutes. Seven patients underwent tolerance of dextrose 10% through the catheter after 12 hours and one 24 hours after the procedures. Enteral feeding was indicated after the dextrose 10% tolerance was performed. No complications re¬lated to the procedure were observed. Discussion. Currently, the gold standard technique to perform a gastrostomy is the percutaneous or endoscopic approach. In patients with head and neck tumors, when it is not possible to insert a nasogas-tric tube to insufflate the stomach, a laparoscopic gastrostomy would be indicated. We describe a new technique, step by step, to perform less invasive laparoscopic surgery by a single port laparoscopic gastrostomy. Conclusion. The diameter created is the same as the one performed with an open tech¬nique, but in this case, with a minimally invasive approach, that allows us to start feeding the patient with a high quality of feeding, because of the wider lumen.
Key words. Gastrostomy, laparoscopy, novel techniques.
Gastrostomía laparoscópica por incisión única: descripción de la técnica y experiencia inicial
Resumen
Introducción. Las primeras gastrostomías para alimentación eran realizadas mediante incisiones medianas supra-umbilicales. Estas técnicas suelen realizarse en enfermos en mal estado general, ya sea por desnutrición o por su causa neurológica o tumoral. El desarrollo de nuevas técnicas logró que la gastrostomía percutánea o endoscópica sean el “gold standard”. Pero ante la imposibilidad de las mismas presentamos una nueva alternativa mediante vía laparoscópica por incisión única. Material y métodos. Entre julio de 2012 y junio de 2013 se realizaron 8 gastrostomías laparoscópicas por incisión única. Cinco correspondieron al sexo femenino, con una edad media de 77 años (rango: 67-87). Resultados. El tiempo medio del procedimiento fue de 45 minutos. Siete pacientes comenzaron tolerancia con glucosa a las 12 horas post-procedimiento y uno a las 24 horas. Posteriormente se indicó alimentación enteral. No se observaron complicaciones relacionadas con el método. Discusión. La técnica “gold standard” es el abordaje percutáneo y/o endoscópico. En pacientes en los cuales no es posible insuflar el estómago o progresar el endoscopio, la gastrostomía laparoscópica por incisión única sería una opción factible. Describimos esta nueva técnica paso a paso para la realización de gastrostomías en forma mini-invasiva mediante laparoscopía por incisión única. Conclusión. La gastrostomía laparoscópica por incisión única es una nueva técnica donde el lumen creado es mayor al de las gastrostomías percutáneas, permite una alimentación de mejor calidad en forma más temprana, tiene baja morbilidad y se obstruye con alimentos y medicación con una frecuencia menor comparada con las técnicas estándares.
Palabras claves. Gastrostomía, laparoscopía, nuevas técnicas.
In the 18th century, John Hunter described for the first time the use of a gastric feeding tube; later on, Sedillot in France, during half of the 19th century, described the first surgical gastrostomy.
The first description of a technique to minimize the trans-parietal access for gastrostomies was described by Harry Fenwick in 1884 and published in the Annals of Surgery, one of the most well known journals in general surgery.1, 14
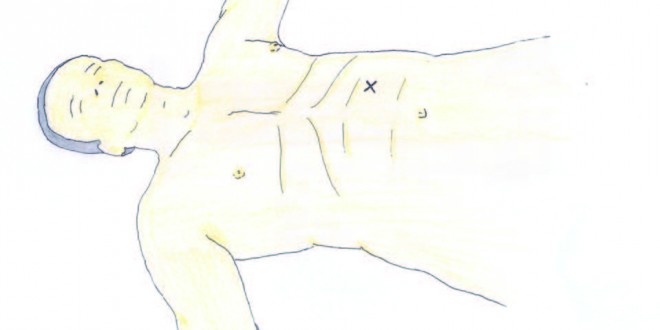
The gold standard technique to perform a gastrostomy is the percutaneous or the endoscopic approach.4, 5, 9 In patients with head and neck tumors when it is not possible to insert a nasogastric tube to insufflate the stomach, a single port laparoscopic gastrostomy would be indicated (Figure 1).17
Figure 1
Material and methods
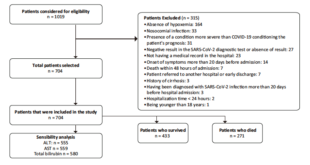
Between July 2012 and June 2013, 8 patients underwent a single port laparoscopic gastrostomy. Five were females and 3 were males. The range of age was from 67 to 87 years old with a mean of 77. All the patients had head and neck tumors with no possibility to get access to the stomach through a nasogastric tube. That is the reason why a percutaneous or endoscopic gastrostomy could not be performed.
This new approach would be indicated in patients with head and neck tumors, head and neck trauma or any other disorder which do not allow the surgeon to pass through the esophagus and reach the stomach to insufflate it and perform a percutaneous gastrostomy (gold standard). In all our patients it was not possible to place a nasogastric tube. Six patients had head and neck tumors with obstruction of the esophagus with 2 or 3 failed tries to inset a tube. The other 2 patients had facial trauma of Le Fort 3 classification with no possibility of passing through the esophagus with the tube. The patients with head and neck tumors were admitted in a regular ward and the 2 patients with trauma were in intensive care unit.
Necessary material
A laparoscopic scope with working cannel, a 10 or 12 mm trocar, light source, optic fiber, pneumoperitoneum insufflator and a grasper.
Surgical technique
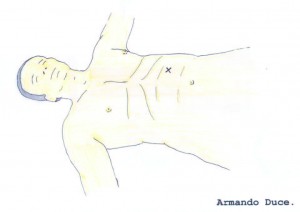
The patient is placed in prone position. Asepsis and antisepsis are carried out from the inter mammillary line to the pubis. An incision is made, two fingers under the costal border (9th rib), from the left trans-rectal and as close as possible to Spiegel’s semilunar line (external attachment of rectus sheath). A 10 mm incision is made in order to place later a trocar (Figures 2 A-B and 3).
The abdominal cavity is entered with an open technique, opening the anterior rectus aponeurotic sheath, blunt dissection of the rectus is performed, avoiding injury of the anterior intercostal nerves, then opening the posterior aponeurosis of the rectus, dissecting the pre-peritoneal fat and opening the peritoneum to get into the abdominal cavity.
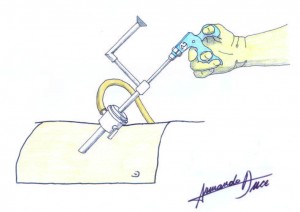
Placement of a 10 mm trocar, carbon dioxide insufflation at 12 mm Hg pressure or less and 20 ml flow, are performed (Figures 4 A-B).
A 30-degree working channel optic is inserted (Figures 5 A-B). Another option is to insert the instruments parallel to the 10 mm trocar, when using regular laparoscopic instruments (Figure 5 C).
The left quadrant is inspected visualizing the left liver lobe, the distal esophagus, stomach and left colon under the sub-phrenic space.
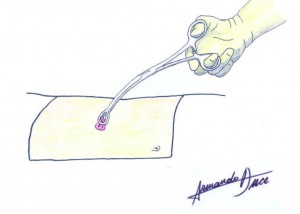
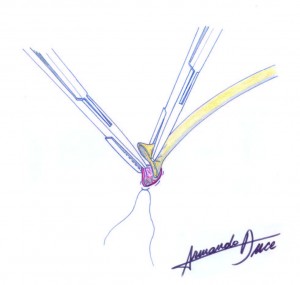
A “grasper” is placed through the optics working cannel or in parallel to the trocar, mobilizing the anterior portion of the stomach; we choose the segment with the appropriate mobility to avoid injury of the gastric vasculature by tension when pulling towards the abdominal wall (Figure 6). This approach uses the gastric antrum to insert the tube.
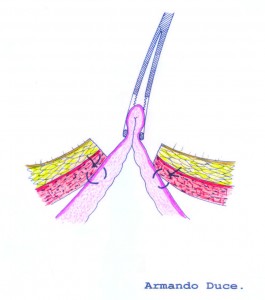
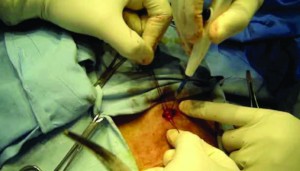
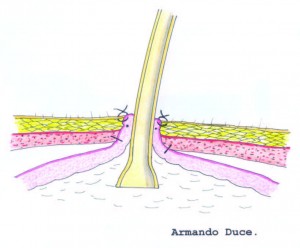
When exteriorizing the gastric segment (antrum), the pneumoperitoneum is lost, and mobility and lack of tension are verified with a Foerster clamp (Figure 7 A-B). The sero-muscular layer of the stomach is fixed with landmark sutures to the aponeurosis of the rectus (Figure 8), then, purse-string sutures are applied around the area where the foramen of the future ostomy will be created (Figure 9). The stomach is then incised (Figure 10), plane by plane, checking its lumen, and a Pezzer tube is inserted inside the stomach. Finally the mucosal layer is closed with purse-string sutures and the sero-muscular wall excess of the stomach is fixed to the cutaneous layer (Figure 11).
Dextrose is instilled with a Boneau syringe, through the Pezzer tube and “clamped” to check passage of the fluid to the duodenum, absence of leaks and reflux when unclamping.
The Pezzer tube is fixed to the skin and cutaneous closure with non-continuous sutures are performed, according to the orifice needed for the tube diameter (Figures 12 A, B, C).
A tolerance of dextrose 10% through the catheter is carried out after 12 hours, and enteral feeding is supplied.
Results
The procedure was performed in all the patients with no technical complications. The mean time of the procedure was 45 minutes. In 7 patients the tolerance of dextrose 10% through the catheter was carried out after 12 hours and in one of them, 24 hours after the procedure. Enteral feeding was indicated in all the cases immediately after the tolerance of dextrose 10% through the catheter was performed.
No complications related with the procedure were observed.
A high quality of feeding was significantly faster when comparing with others techniques, because the thickness of the tube is bigger in the single port laparoscopic gastrostomy. Nutritionists are in charge of the feeding and it is well known that the bigger the diameter is, the better the quality of feeding. This could be an advantage of this approach.
Discussion
Many options have been described to place a tube into the digestive tract for decompressing or feeding purposes.2
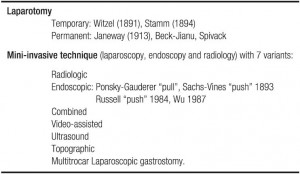
They can be classified as follows in table 1:
Table 1. Gastrostomies classification.
Since the first classic descriptions of surgical gastrostomies for feeding or decompression purposes by a supra-umbilical incision, patients were operated under general anesthesia, with prolonged time of surgery, these were patients with poor health status, undernourished due to inadequate intake for neurological or tumor disorders, with prolonged hospitalization, both for the recovery of the intestinal motility as well as for the recovery of post-surgical wounds.15, 16 The issues of total recovery time to allow the patient an earlier return to normal activities, of the complications due to the procedure and the economic cost have urged to find a better surgical option to create new techniques to maintain feeding continuity in this group of patients, with unmet basic caloric requirements and no parenteral alternative.
The technique to introduce a tube orally, to insufflate the stomach and exteriorize it to construct a definite ostomy, as described by Hendrick, has evolved in time: radiology contributed with a new device with the introduction of the Seldinger technique for percutaneous gastrostomies improving surgical time, type of anesthesia, less invasion of the abdominal wall, improving hospitalization stay and recovery, both inside and outside the hospital, reducing costs and constituting a simpler approach to be learnt and practiced by the community of surgeons.7, 8, 10, 11 The new techniques are not exempt of morbidity and mortality, but are significantly reduced.
The introduction of laparoscopy as a new technique was a turning point, as it allowed to explore the abdomen and operate with trocars, with the same advantages of minimally invasive techniques: it allowed to insufflate the stomach and displace it from the surgical field away from the abdominal wall to the colon, for it has been the cause of some complications in radiological-guided percutaneous procedures. In this way, with the use of five trocars, which eventually became three, and with the pneumoperitoneum and optic fiber, the surgical technique was improved.3, 6 The advantage of this technique is that there is no need to pass through the aero-digestive tract to reach the stomach, since it is approached from the abdomen under direct visualization of the intra-abdominal organs.
An endoscopic gastrostomy is another option to reduce the number of incisions and use of pneumoperitoneum.12, 13, 16 As this procedure requires patent passage to the stomach and uncontrolled gastrostomy fixation to the abdominal wall with no possibility to visualize interposing structures, it was necessary to devise hybrid laparoscopic endoscopies to minimize the number of ports utilized.
Under these circumstances, it was necessary to be very selective on the segment chosen for the ostomy that would allow a faster recovery after the gastrostomy in patients unable to progress through the upper digestive tract. Therefore, adhesions had to be minimized considering future intra-abdominal procedures, with the advantages of minimally invasive procedures such as less post-operative pain and faster recovery, thus enabling earlier feeding. Following all these parameters a single incision is done placing the trocar in a single working channel, under laparoscopic standards, with direct visualization, minimum pneumoperitoneum and completing the technique with a gastric fixation and ostomy from outside of the abdominal wall.
In the surgical options to perform a gastrostomy there are: open, endoscopic, laparoscopic, percutaneous and combined procedures, but when considering minimally invasive procedures for shorter surgeries, there are patients who are unable to pass the esophagus and undergo endoscopic or percutaneous procedures, but who need a quick intervention with less abdominal trauma, in them, open procedures are ruled out. The technique we herein introduce came about when thinking on the need to have a laparoscopic technique, with three trocars and shorter surgeries of approximately one hour and pneumoperitoneum.
Based on this information, we designed this procedure tailored to the patient’s needs according to the pathology, with a single left para-rectal incision and placement of a single trocar and optics with working channel, with full vision to explore the abdominal cavity and look for metastases and eventually take selected biopsies under direct visualization of the gastric segment in which the gastrostomy shall be created. It is necessary to control the pressure on the abdominal wall by the final positioning and abdominal pneumoperitoneum time (approximately 15 minutes), gastric control during wall fixation and confirming that only one portion of the stomach has been utilized for the gastrostomy considering future surgeries. Costs are low, especially hospitalization costs and rapid recovery from mini-invasive procedures, with minimal procedure related functional digestive disruption.
In summary, one of the main advantages of having a bigger lumen is that the feeding can be instituted with regular formulas but also with formulas rich in fibers, which allows as a better quality of feeding. Another advantage is that the medication can be given through the same ostomy with less obstruction problems. The obstruction of the tube is a serious complication in these patients because many times the patients have to be taken to an institute or hospital to solve the problem. And during this time the patients cannot be fed.
Conclusions
The main advantage of this technique is that feeding of the patient starts with the bigger lumen when comparing with other techniques, something not achieved up front with other minimally invasive techniques. The lumen created is the same as with the open techniques but with all the benefits of the minimally invasive approach. Therefore, the single incision laparoscopy prevents injury to the abdominal wall, with all the advantages of laparoscopic surgery, and allowing starting feeding sooner with a large lumen ostomy, providing high quality feeding without waiting months to achieve this lumen, as is the case with the other techniques.
Conflict of interest. Mariano Palermo, Mario Luis Domínguez, Pablo Acquafresca, Guillermo Duza and Mariano Gimenez have no conflicts of interest or financial ties to disclose.
Reference
- Fenwick H. A successful case of gastrostomy for aphagia due to malignant disease of the pharynx and fauces. Ann Surg 1885; 1: 342-345
- ASPEN Board of Directors and the Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. J Parenter Enteral Nutr 2002; 26: 1SA-138SA.
- Arnaud J, Casa C, Manunta A. Laparoscopic Continent Gastrostomy. Am J Surg 1995; 169: 629-630.
- Brady A. Percutaneous gastrostomy: US guidance for gastric puncture. Radiology 2000; 214: 303-304.
- D’Agostino HB, Wollman B. Percutaneous Gastrostomy. A Radiological Alternative? Radiology 1996; 623: 625-626.
- Edelman D, Unger S, Russin D. Laparoscopic Gastrostomy. Surgical Laparoscopy and Endoscopy 1991; 1: 251-253.
- Ferguson DR, Harig JM, Kozarek RA, Kelsey PB, Picha GJ. Placement of a feeding button («one-step button») as the initial procedure. Am J Gastroenterol 1993; 88: 501-504.
- Foutch PG, Talbert GA, Gaines JA, Sanowski RA. The gastrostomy button: A prospective assessment of safety, success, and spectrum of use. Gastrointest Endosc 1989; 35: 41-44.
- Giménez M, Suárez Anzorena F, Cerisoli C. Gastrostomía percutánea: variantes técnicas. Rev Argent Cir 1999; 76: 106-112.
- Halkier Bk, Ho Cs, Yee Can. Percutaneous feeding gastrostomy with the Seldinguer technique: review of 252 patients. Radiology 1989; 171:359-362.
- Lee MJ, Saini S, Brink JA, Morrison MC, Hahn PF, Mueller PR. Malignant small bowel obstruction and ascites: not a contraindication to percutaneous gastrostomy. Clinical Radiology 1991; 44: 332-334.
- Russell T, Brotman M, Norris F. Percutaneous endoscopic gastrostomy: A new simplified and cost-effective technique. Am J Surg 1984; 148:132-137.
- Sánchez RB, van Sonnenberg E, D’Agostino HB, Goodacre BW, Moyers P, Casola G. CT guidance for percutaneous gastrostomy and gastroenterostomy. Radiology 1992; 184: 201-205.
- Stamm M. Gastrostomy: A new method. Med News 1894; 54: 324-326.
- Vitcopp GM, Fernández Marty AP. Vías de alimentación enteral por cirugía mini-invasiva. Actualización en Nutrición 2004; 5: 17-23.
- Wollman B, D’Agostino HB, Walus-Wigle JR, Easter DW, Beale A. Radiologic, endoscopic and surgical gastrostomy: an institutional evaluation and meta-analysis of the literature. Radiology 1995; 197: 699-704.
- Palermo M, Giménez M, Gagner M. Laparoscopic Gastrointestinal Surgery. Novel techniques, extending the limits. AMOLCA Editorial. In Press.
Correspondencia: Mariano Palermo
Av Pte Perón 10298 Ituzaingo (CP 1714), Buenos Aires, Argentina
Tel: 5411-44819995
Correo electrónico: palermomd@gmail.com
Acta Gastroenterol Latinoam 2015;45(4):280-287
 Revista ACTA Órgano Oficial de SAGE
Revista ACTA Órgano Oficial de SAGE